Ultimate Guide to Hiring a Credentialing Service
Everything a practice owner, clinic director, or independent provider needs to evaluate, select, and onboard the right credentialing partner—so you can go in-network faster, avoid denials, and protect cash flow.
Jump to mini-navigation ↓Hiring a credentialing service the right way
Credentialing is how payers verify a provider’s qualifications (licenses, education, malpractice coverage, employment history) before issuing a contract. Done well, it compresses timelines, reduces rework, and prevents costly revenue gaps. Done poorly, you’ll face “development” requests, lost months, and avoidable denials. This guide shows you how to select a partner who understands both credentialing workflows and the downstream revenue cycle—and how to structure the relationship for measurable outcomes.
At RxCredentialing, we streamline the continuum: NPI → CAQH ProView → Medicare (PECOS/CMS-855) → commercial payer enrollment → contracting → RCM handoff with eligibility, prior auth, clean claims, and denial prevention. Explore our credentialing services, or skip ahead to the onboarding checklist.
Why hire a credentialing service (instead of doing it in-house)?
Speed and expertise
- Pre-built templates for payer applications and CAQH attestation.
- Knowledge of panel status, fee schedule requests, and negotiation windows.
- Rapid response to “development” notices to avoid resets.
Lower total cost
- Avoid hiring/training a full-time FTE for fluctuating workload.
- Prevent delays in go-live that postpone revenue.
- Reduce denials with front-end accuracy.
Tip: Pair credentialing with RCM setup to ensure eligibility, EDI/ERA, and payment posting are live on day one.
When to hire (and when to wait)
Hire when you’re starting a new clinic, adding locations, expanding payer mix, experiencing backlogs, or facing critical renewals. Wait if you’re mid-audit without docs ready—first tighten your records using our credentialing checklist and FAQ.
| Scenario | Hire now | Reason |
|---|---|---|
| New practice | Yes | Compress NPI → CAQH → Enrollment timeline; hit launch targets. |
| Adding providers | Yes | Parallelize CAQH, licensing, payer apps; standardized intake. |
| Contract renegotiation | Yes | Coordinate contracting and effective dates. |
| Single payer issue | Maybe | Isolated repair vs full outsourcing—depends on volume and timeframe. |
| Incomplete documents | Wait | Fix document gaps first (malpractice, license, W-9) via enrollment support. |
Evaluation criteria: how to compare credentialing vendors
1) Domain depth
Do they handle Medicare PECOS, CAQH, revalidation, and commercial panels across states and specialties?
2) Process & tools
Structured intake, trackers, ticketing SLAs, and secure document storage. Ask for their intake packet and sample status report.
3) RCM awareness
Credentialing choices should support eligibility, auths, and claims—not conflict with them.
4) Timelines
Honest estimates by payer; weekly reporting; clear “development” handling.
5) References & outcomes
Look for case studies, time-to-effective-date metrics, denial reduction, and first-pass yield improvements.
Explore our credentialing, contracting, and state licensing pages for detailed scope.
14 vendor questions you should always ask
- What payers and states do you credential most often for our specialty?
- How do you build and maintain CAQH profiles and manage 90-day attestations?
- Do you handle PECOS CMS-855 and revalidation?
- How do you track timelines and escalate “development” requests?
- What’s included vs. out-of-scope (e.g., prior auth, eligibility)?
- How do you secure PHI and control access?
- What are your standard SLAs for response and follow-ups?
- Do you assist with contract negotiations or just credentialing?
- How do you coordinate with our EHR/RCM vendor?
- What % of applications are approved on first submission?
- What’s your approach to panel closures and waitlists?
- How do you coordinate effective dates with marketing/launch?
- What onboarding documents do you require from us?
- What is the communication cadence and reporting format?
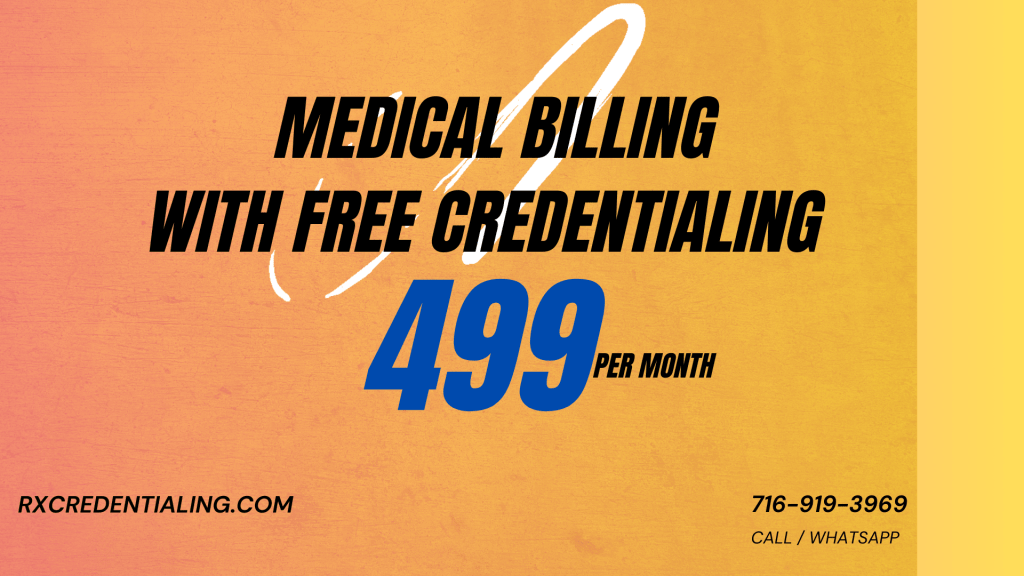
Credentialing pricing models (and how to compare apples to apples)
| Model | Best for | Watch outs |
|---|---|---|
| Per-payer flat fee | Predictable provider additions | Confirm what’s included (CAQH, Medicare, revalidation). |
| Bundle (credentialing + contracting) | New practices & multi-payers | Ensure fee schedule requests are explicit in scope. |
| Monthly retainer | Ongoing maintenance & re-cred | Define ticket caps, SLAs, and reporting. |
| RCM-aligned package | Full launch support | Clarify RCM responsibilities vs credentialing team. |
We provide transparent quotes on Get Started and scope alignment via discovery call.
Red flags that cost you months (and money)
- “Guaranteed approval dates.” (Payers control timelines.)
- No written scope or SLA; vague deliverables.
- Doesn’t manage CAQH attestations or expirables.
- No plan for re-credentialing and Medicare revalidation.
- Weak PHI security and unclear data retention.
- No integration with RCM workflows.
Onboarding checklist: what your vendor should collect on day one
Provider & entity
- License(s), state licensing status, DEA (if applicable)
- CV, education, training, board (if applicable)
- W-9, EIN, legal name, taxonomy codes
- Malpractice face sheet; policy limits/dates
Systems & payer data
- NPI Type 1/2 confirmation
- CAQH access & 90-day attestation plan
- PECOS account and CMS-855 status
- Target payers and practice locations
- EDI/ERA enrollment plan with RCM
Download a consolidated list in our Resources center or talk to our enrollment team.
KPIs & SLAs that actually predict cash flow
| Metric | Target | Why it matters |
|---|---|---|
| Time to submission | < 7–10 business days | Faster filing → earlier effective date. |
| Development response time | < 48 hours | Prevents resets & stalls. |
| Approval rate on first submission | > 90% | Data hygiene & process quality. |
| Re-credentialing on-time rate | 100% | Avoids terminations and cash gaps. |
| RCM readiness at go-live | 100% | Eligibility, auths, EDI/ERA, posting ready. |
We report these KPIs weekly. See FAQ and Contact for details.
Compliance & security (non-negotiables)
Your vendor will handle sensitive PHI/PII and payer credentials. Require: encrypted storage, role-based access, documented incident response, least-privilege accounts, and secure file exchange. Establish your shared operating picture with a single “source of truth” for identity, addresses, taxonomy, and contact details to keep CAQH, PECOS, and payer applications perfectly consistent.
Need a second opinion? Our team can audit your existing setup and hand you a prioritized remediation plan. Start here: Get Started.
Switching vendors without losing momentum
- Export everything: CAQH printouts, PECOS records, payer application receipts, open developments, and contact lists.
- Centralize data: standardize legal names, addresses, and taxonomies; align with FAQ guidelines.
- Prioritize re-credentialing: anything due within 90 days goes first.
- Rebuild the master tracker: every payer, status, next action, and target effective date.
- Launch a weekly cadence: KPIs and blockers review (see KPIs & SLAs).
We do white-glove transitions—learn more about credentialing, contracting, and RCM.
Ready to hire a credentialing partner you can measure?
We handle enrollment, contracting, and RCM readiness—so you bill sooner and cleaner.
Hiring a credentialing service: FAQ
How long will credentialing take with a vendor?
Plan for 60–120 days for common commercial payers and 30–90 days for Medicare via PECOS—assuming complete documents and timely responses.
Do they also handle contracting?
Some do, some don’t. We offer payer contracting with fee schedule requests and effective-date planning.
What should be in the scope?
Provider intake, CAQH build & attestation, Medicare PECOS/CMS-855, commercial applications, development responses, and re-credentialing tracking. Optional: RCM readiness.
Will this reduce denials?
Yes—front-end accuracy lowers eligibility/contracting mismatches. Pair with eligibility and denial prevention.
How do we get started?
Share your provider roster and target payers via Get Started, or book a discovery call.
Helpful RxCredentialing resources
Home • About • Credentialing • Provider Enrollment • CAQH • PECOS • Payer Contracting • RCM • Eligibility • Prior Auth • Payment Posting • Appeals • Denials • Behavioral Health & Rehab • State Licensing • Resources • Blog • FAQ • Get Started • Contact
We would love to hear from you.
Contact Us
Have a question or want to learn more about our services? Fill out the form below and our team will get back to you within 24 hours.
We serve all 50 states.