"You don't have to be great to start but you have to start to be great"
What you will learn from this read?
Starting your own telemedicine practice in the United States can seem like a formidable task, particularly if you’re lacking the necessary information.
However, equipped with the right knowledge and resources, you can successfully embark on this journey without even needing to quit your current job.
Together, we’ve assembled a comprehensive, step-by-step guide that aims to simplify this process for you.
This guide serves as a valuable resource for various medical professionals such as licensed physicians, MDs, DOs, nurse p
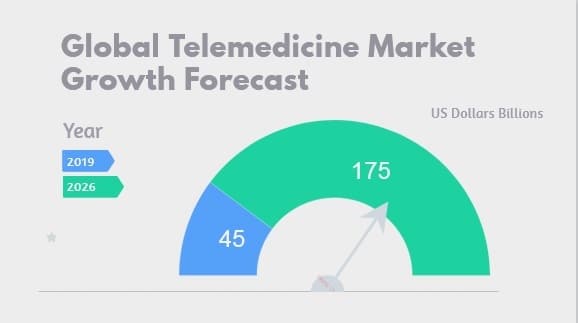
But before we delve into the details of starting your business, let’s first explore the rapid expansion of telemedicine or telehealth and understand its impact on existing and new medical businesses. By grasping the “why” behind telemedicine’s growth, we can more effectively navigate the “how” of beginning your very own telemedicine practice.
Why Telemedicine?
The remarkable benefits of telemedicine cannot be overstated. As a physician, it offers you the fantastic opportunity to engage with patients more conveniently and inexpensively.
Just imagine the liberation of not needing to expand your clinic, hire additional staff, or lease a new office – all while successfully advancing your practice.
This innovative medical approach allows you to reach more patients, without the necessity of leaving the comfort of your home or office.
Moreover, the ascendancy of telemedicine doesn’t stop at convenience alone. An exciting new reality is rapidly unfolding – telemedicine is leading the way into the future of medical practice.
A glance at the following statistics will illuminate the sheer impact and potential of this cutting-edge trend.
What is Telemedicine?
Telemedicine or telehealth is a branch of medicine where healthcare providers can communicate with their patients using a two-way audio and video gateway.
Telemedicine or telehealth is an interchangeable term that is used for the provision of distant health services.
Telemedicine can also be defined as “attending patients remotely with help of HIPPA compliant software through audio or video call where the doctor and the patients are located at different locations”.
The doctors communicate with patients through an audio or video device and ask them questions in order to get more understanding of the situation.
It is convenient for the patients as they can explain their condition without leaving home.
How is it beneficial?
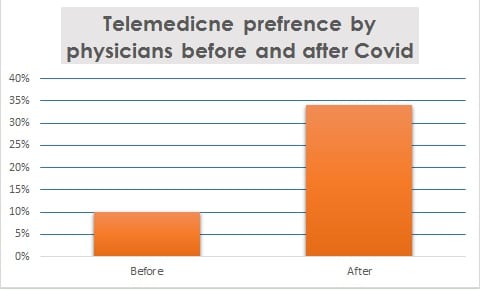
Since March 2020, It is being practiced in every part of the world, especially in the United States.
Medicare, Medicaid, Tricare, and many other commercial insurance plans has asked its providers to provide care via telehealth to avoid patients exposure to COVID-19.
Telehealth was not that much known nor it was being practiced before Covid-19.
Medicare, Medicaid and few other healthcare insurances were only covering it for rural areas or where patients had limited access to specialists.
Reimbursements to providers for telehealth services were very low as compared to what these healthcare insurance companies normally pay providers in an office setting.
Due to social distancing and wide spread of Covid-19, Government of United States, CMS and HHS has asked every insurance payer to allow providers to offer telehealth services.
The payers have been also asked for 100% reimbursements to providers for telehealth services.
Telemedicine has made survival easier for new startups as it’s an opportunity to build healthy revenue at lesser expense.
It can deliver care more efficiently for elders, kids as well patients with chronic conditions.
It is the best solution for under-served health care areas.
It also increases patient to physician communication which overall improves health.
It also helps in improving patient data sharing process, which enhances coordination among physician in order to diagnose reliably.
How Telemedicine Services are classified?
Currently, the telemedicine services can be classified into three categories.
First: where a patient and doctor interact with each other with the HIPPA-compliant software, this interaction can be audio or video through audio call or video call, it is called Interactive Medicine.
Second: This is called Store and Forward, where one physician can forward patient’s information to another practitioner in another location.
For example, a primary care physician has obtained the basic information, has seen the patient in person, collected all required information along with results of the medical tests required to support diagnosis.
After reviewing all this information the specialist can advise the treatment.
Third: Patient Monitoring services where the caregivers monitor a patient residing at their home and they check different data such as blood sugar or blood pressure with use of various Telemedicine devices.
Boring…., Yes I know, You already know what I expressed above however I just tried to build a background in order to convince you that why you should take this telehealth business opportunity seriously.
Now, it’s time to dive deep to know Each Single Step you need to accomplish in order to start your own Telemedicine Practice from Scratch.
Key steps to set up a telemedicine practice successfully.
- Medical Board Certification (Optional).
- Medical Licensing
- NPI.
- EIN.
- Office Space & Address.
- Bank Account.
- Medical Malpractice.
- DEA Registration (Optional).
- Provider Enrollment and Credentialing.
- HIPPA Complaint Audio Video Software.
- Medical Billing.
- Collaborative & Supervising Physician (Optional).
- Practice Marketing & Re-Targeting.
- The Good News.
Medical Board Certification.
Medicare and commercial healthcare payers in United States have made it mandatory for Nurse Practitioners to have a board certification.
The certificate should be from any recognized board in order to enroll and practice medicine. This also applies to telemedicine or telehealth.
It is not required by physicians in most cases, but it varies state to state and payer to payer.
If you are a Nurse practitioner. You must get board certification from AANP or any other accredited agency.
The board certification is not mandatory for other specialties except for Nurse Practitioners.
Medical Licensing to start your own practice.
To setup your own telehealth practice in any state you will need a state medical license. You can get your state license from any licensing service agency.
You need to be licensed in the state where you are planning to practice telehealth or telemedicine.
Licensing takes anywhere from 2 to 6 months but due to Covid-19 and public health emergency many states have waived the license requirements and some states are also issuing temporary licenses which only takes 7 to 14 days in most case.
You can also Contact Your State Medical Board directly to find out more.
If you are not familiar with licensing process, you can get FREE ADVICE here from our experienced team.
National Provider Identifier (NPI).
You can apply for your National Provider Identification Number online.
You can also contact us to apply for your NPI Free of cost as we do not charge anything for NPI setup.
To get your FREE NPI number just write us a message by filling the contact form given at the end of this article.
You can apply for your National Provider Identification Number online.
You can also contact us to apply for your NPI Free of cost as we do not charge anything for NPI setup.
To get your FREE NPI number just write us a message by filling the contact form given at the end of this article.
Employer Identification Number (EIN).
Practicing telemedicine will also require an EIN, if you are planning to operate as a business entity.
If you are an individual and does not want to practice as a medical business company then you can use your SSN or get an EIN as a sole-proprietor.
If you already have an EIN but you lost the EIN confirmation letter received from IRS. Here is an easy way to get copy of EIN confirmation letter.
To Obtain an EIN, all you have to do is either call IRS and request over the phone or visit their website and complete few simple steps to file your EIN application.
It only takes up to 7 days to get the EIN.
Office Space & Address.

A lot of people don’t go for their own telehealth practice setup because they think that they would need an office but actually they don’t.
Everyone does not need to set-up an office to have a telehealth practice however having an office is an advantage if you want to do it on big scale.
However if you have just started and you are cost conscious then you don’t need it, to start your own telehealth practice.
You can use your home address instead wherever its required.
The best part is that telemedicine doesn’t require patients to visit physician location therefore you can use your home address for the sake of administrative tasks.
Business Bank Account.
The next step is to have a business bank account. If you don’t have a tax ID from IRS then You can not open a bank account.
But You can have an individual bank account by using your social security number.
You can use your personal bank account to receive direct deposits from insurance payers as Medicare does not prefer to send checks. Here is our guide to setup Medicare direct deposit instructions for your medical practice.
Medicare prefer direct deposit or transfer money into your bank account.
This makes practice administration easier as you don’t need to allocate time to manage checks from insurance payers.
Most of the insurance payers require to set up a direct deposit facility.
Direct deposit setup also referred as EFT setup is beneficial as you will get your money right into your bank account.
Our team can help you to create EFT Setup, do write us if you have any question regarding your EFT setup.
Medical Malpractice Insurance.
To set up a telemedicine practice in any fashion you are required to carry a professional liability insurance that has 1 million to 3 million coverage as per the criteria set by most of the healthcare insurance payers.
A Malpractice insurance policy can cost anywhere from $1000 to $2000 for NPs, and $3000 to $5000 for Physicians.
I have dedicated article on Medical malpractice insurance to help you understand it well.
There are two type of Coverage for medical malpractice insurance.
- Claim based coverage.
- Occurrence based coverage.
We recommend Occurrence based coverage which is usually expensive.
There are many medical Malpractice Insurance providers. Some are cheaper, some are expensive based on their offer.
The key consideration here is that you just need a policy to qualify your eligibility for all the insurance payers, you are planning to Enroll or Credential with.
We can definitely help you to choose Malpractice provider depending upon your specialty.
For Nurse Practitioners, we always recommend CM&F Group, we can get your malpractice coverage in 30 minutes from CM&F group in case you find it difficult.
DEA Registration.
You will need Drug Enforcement Administration number if you will prescribe any drugs falling under controlled substance regulations.
Provider Enrollment & Credentialing.
Physician insurance credentialing can take from two to four months.
We always recommend that you go with Medicare credentialing first.
Due to the fact that you can treat Medicare patients without having a medical malpractice insurance policy.
Therefore Credentialing with Medicare first helps you save cost and generate revenue by treating patients.
Once you start making some extra money you can go for medical malpractice insurance and get credential with other insurance payers.
Once you are credentialed with 15 to 20 insurance payers in your state. You would be listed on the websites of those payers as their In-network medical provider.
Therefore if you are a full time PCP. The medical insurance payer will assign you a panel of up to 400 patients.
That’s all you need to generate healthy revenue to expand your own telehealth practice.
If you are not PCP but a specialist. You will be still listed on the websites of all the insurance payers with whom you have credentialed as a specialist provider.
Furthermore PCPs of all those insurance payers will refer their patients to you. If they require services in your specialty.
Therefore it’s worth getting enrolled with all those insurance payers. This will definitely increase your patient volume.
Cost for telemedicine credentialing services:
Telemedicine credentialing companies can charge you from $200 per payer per provider.
Some telemedicine credentialing companies also offer flat rate for multiple payer enrollment such as $1000 for 10 insurance payers to $2000 for 18 to 20 payers.
In order to build a strong telemedicine business and maximize your chances to welcome more patients, $2,000 is not a bad deal.
Spending USD 2,000 to get enrolled with 18 to 20 payers increases your patient volume to maximum.
If you are planning to higher many medical providers for your telemedicine business.
Telemedicine credentialing costs can be minimized by outsourcing. It also helps to concentrate on your activity.
The right physician credentialing company takes ownership for every task from payer analysis to EFT setup in order to receive reimbursements directly to your bank account.
Setting up your telehealth practice is much better than working for someone because with the passage of time your brand will grow much faster than your monthly salary.
HIPPA Compliant Audio Video Software.
During public health emergency, CMS has allowed health care providers to practice Telehealth in any way that is available.
You no longer have to worry about Telehealth platform requirements as you can provide these services’ via Skype, Doxy, WhatsApp , FaceTime etc.
If video call is not possible you can also provide care using audio calls.
You can provide these services to both existing and New patients.
You can also give an eye to below given option.
Medical Billing.
Once you start treating the patients. You will need to have a medical biller to submit claims to insurance payers for reimbursement.
You can also outsource medical billing as this will enable you to allocate more time and concentration on core activity.
Outsourcing medical billing enables you to streamline your cash flows fast.
The expertise of medical billing company will speed up claim processing. It will also help you to keep claim denial rate to minimum.
There are many companies who charge from 3 to 5 percent of the monthly collection of medical practice.
Some even charge a flat rate such as $500 for $10,000 collection and $5,000 for $100,000 collection.
Collaborative & Supervising Physician.
Nurse practitioners find it challenging to set up telemedicine due to the requirement of a collaborative physician.
However, there are Twenty Two States where you don’t need a collaborative physician at all, you can practice 100% independently if you are in any of those 22 States.
Furthermore, there are 13 States where you just need an agreement with one of the supervising physician.
That means the supervising physician could be anywhere in the state.
Normally its recommended that collaborative physician should be in the area of 30 miles of your practice area or of your home address.
In some States you need a supervising physician to be working with you at the same practice.
If you are in any of these States don’t think again to have your own telehealth practice without having a supervising physician.
So if you are from those States where you need a collaborative physician, you are always welcome to write us at support@rxcredentialing.com.
We provide best physician management consulting services and you can ask us anything without paying anything as we don’t charge for sharing the best advice for you.
Collaborative physician doesn’t have to be present with you, you can practice independently.
All you need to have is an agreement saying that you have a supervising physician who reviews your chats from time to time to see that you are on right track.
If you are planning to set up telemedicine practice in a state where they require a supervising physician to be present at the same practice.
In that case better option is to find the supervising position who is also willing to partner with you.
This will help to align the interest and build long term relationship.
Marketing Your own telemedicine practice.
Now it’s time to strategize your marketing.
Being a startup you can initiate your marketing campaign from social media.
You should create your business pages for Facebook, Instagram & Pinterest or on other platforms to inform your social connections about your Telemedicine practice.
Start sharing valuable tips, precautions or other related stuff to help people build healthy lifestyle in your specialty. This will increase your followers and your message will also be spread by word of mouth.
Starting your own telemedicine practice – Another Way
Good news for you is that if you are working somewhere then you already have most of the requirements such as medical license, malpractice insurance, board certification, NPI, EIN, home or office address and a bank account.
Therefore, You can easily start your Telemedicine or telehealth practice.
With the passage of time you will be able to conclude if your practice is growing, should you invest more in marketing and clarify many more doubts you may have at start.
Lastly, do check our guide on starting your medical practice as physician assistant.
Do share your feed back at support@rxcredentialing.com, we would love to hear form you as well as answer your questions regarding above stated steps to enable you to start your own successful telehealth practice.
Faqs
What is telemedicine?
Telemedicine is a branch of medicine where healthcare providers communicate with patients using audio and video technology, allowing for remote consultations.
Why is telemedicine growing rapidly?
Telemedicine has experienced rapid growth due to its ability to provide convenient and accessible healthcare.
How can telemedicine benefit healthcare providers?
Telemedicine enables healthcare providers to see more patients, reduce expenses, and provide care without physical office space or hiring additional staff.
What are the different types of telemedicine services?
Telemedicine services can be classified into three categories: interactive medicine, store and forward, and patient monitoring.
Do I need medical board certification to start a telemedicine practice?
Medical board certification requirements vary depending on your specialty and state.
Do I need a medical license to practice telemedicine?
Yes, you will need a state medical license in the state where you plan to practice telemedicine.
How do I obtain a National Provider Identifier (NPI) for my telemedicine practice?
You can apply for an NPI online or seek assistance from organizations that offer NPI setup services.
What is an Employer Identification Number (EIN), and do I need one?
An EIN is a unique identification number for businesses. If you plan to operate as a business entity, you will need an EIN.
Can I use my home address as the office address for my telemedicine practice?
Yes, you can use your home address for administrative purposes in a telemedicine practice.
Do I need medical malpractice insurance for my telemedicine practice?
Yes, it is essential to carry professional liability insurance with coverage ranging from 1 million to 3 million.
How do I obtain DEA registration for prescribing controlled substances in telemedicine?
If you plan to prescribe controlled substances, you will need to register with the Drug Enforcement Administration (DEA).
What is provider enrollment and credentialing, and why is it important for telemedicine?
Provider enrollment and credentialing involve becoming an in-network provider with insurance payers, allowing for reimbursement. It is important for establishing relationships with payers.
What software do I need for HIPAA-compliant audio and video consultations?
During the public health emergency, various platforms like Skype, Doxy, WhatsApp, or FaceTime can be used for telehealth. Choose a platform that meets HIPAA compliance standards.
How should I handle medical billing for my telemedicine practice?
You can hire a medical biller or outsource billing services to handle claims submission and ensure proper reimbursement from insurance payers.
Do I need a collaborative or supervising physician for my telemedicine practice?
The requirement for a collaborative or supervising physician varies by state and specialty. Check the regulations in your state.