Medical Billing Services
for Small Practices
Accelerate your cash flow with a billing team that works like an extension of your practice—not a third-party vendor. We submit your claims daily, verify every detail before submission, and maintain a 99% first-pass acceptance rate so you get paid faster with fewer delays.
- ✓ 99% First Pass Rate
- ✓ Daily Claim Submission
- ✓ We Work With All EHR Systems
- ✓ No Long Term Commitment
- ✓ Pay Only 3 to 5% of Collections
- ✓ Real Time Reporting
STARTING FROM
Every Step of Your Billing Process Managed for You
Our team manages the entire billing process for you, including claim preparation, scrubbing submission, tracking, and denial resolution. With proven workflows built for small practices, we help you improve cash flow, reduce errors, and maintain complete visibility into your revenue at every step.
- Encounters Review
- Claim Preparation
- Coding Accuracy Review
- Batch Claim Submission
- Real Time Status Tracking
- Weekly Follow Ups
- Denial Resolution
- Accounts Receivable Management
- EDI, ERA and EFT Setup
- Support for All EHR Systems
What Sets Us Apart
We work directly within your existing EHR and billing system so your workflow stays uninterrupted and your practice never needs to switch software. As soon as your chart notes are signed, we enter them into our shared tracking system, giving you complete visibility from day one. You can see which claims are pending, which were paid on the first attempt, how much was allowed and paid, and where any denials occurred along with clear guidance on how to prevent them in the future. Our transparent approach keeps you informed at every step and ensures you always understand the status of your revenue.
Accurate Coding and Scrubbing
Every encounter is checked for proper coding and complete documentation to reduce errors and prevent denials.
Real Time Claim Tracking
You get full visibility into each claim from the moment notes are signed until payment is posted.
Denial Management
Denied claims are corrected, resubmitted, and followed through until they are fully resolved.
Accounts Receivable Management
Outstanding and aged claims are worked consistently so no payable revenue is ever missed.
A Full Billing Team Behind You
You receive support from an entire billing team rather than a single biller.
Fast and Reliable Communication
You receive responses within hours, not days, so your questions and concerns are handled quickly.
Payer Rules and Compliance Guidance
We keep you updated on payer guidelines and insurance requirements through regular check ins.
Front Desk Eligibility Support
We help your staff with eligibility, benefits questions, and patient responsibility estimates.
Who We Serve
We support healthcare providers across all specialties and practice sizes. Whether you are a solo practitioner, a telehealth based practice, a growing multispecialty group, or a larger healthcare organization, our team delivers complete end to end billing support tailored to your workflow.
Solo and Independent Providers
We handle your entire billing workflow so you can focus on patients. Perfect for providers who want clean claims, fast payments, and support without hiring in-house billing staff.
Telehealth and Hybrid Practices
Telehealth billing requires careful attention to payer rules, state specific requirements, and detailed documentation standards. We guide you through each of these elements and manage the process for you to ensure accurate and compliant reimbursement for every visit.
Multispecialty and Integrated Care Clinics
Multispecialty practices require precise handling of coding rules, modifiers, revenue codes, and taxonomy based billing. We manage these details accurately and ensure each claim is billed under the correct NPI and compliant structure so you can receive timely reimbursement.
How It Works
We follow a streamlined billing workflow designed for speed, accuracy, and zero downtime. Our onboarding process is completed within three to five days, allowing your practice to continue operating without interruption.
Data Collection
We gather essential practice details, provider profiles, and payer mix information to understand your billing structure clearly.
Credentialing Verification Review
We review your payer mix and confirm that each provider is credentialed correctly to avoid any interruptions in reimbursement.
EHR System and Provider Setup
We log into your EHR, add all billing and rendering provider details, and configure your system for accurate claim creation.
EDI and ERA Setup Confirmation
We confirm that all EDI and ERA connections are active so claims flow smoothly and payments are posted quickly.
Charge Master and CPT Code Setup
We create or refine your charge master with the correct CPT codes, fee schedules, and billing rules for clean claims.
Daily Operations Begin
Once everything is in place, our team starts your day-to-day billing workflow including claim preparation, submission, tracking, and follow up.
Have Other Questions? Get in Touch
Our team is here to help you understand every part of the billing process, from claim submission to reimbursement. Whether you need clarity on workflows, payer rules, or how our services fit your practice, we make the entire experience simple, transparent, and stress-free.
Our onboarding process is completed within 3–5 business days, provided all required information is supplied.
Yes — we support all major outpatient specialties including primary care, specialty clinics, mental health, telehealth, rehab therapy, and more.
Yes — we work with nearly all popular platforms such as Tebra, OfficeAlly, eCW, Athena, DrChrono, AdvancedMD, SimplePractice, ICANotes, Optimantra, and more.
Our base plan starts at $499/month and includes free credentialing for solo practitioners. Standard billing plans are 3–5% of insurance collections.
Yes — we offer free credentialing, CAQH maintenance, and revalidation support for billing clients.
All PHI is handled in accordance with HIPAA requirements. Our team uses secure, encrypted systems for file storage, communication, and data access. Access to PHI is limited to authorized staff only, based on job responsibilities, and all activity is monitored.
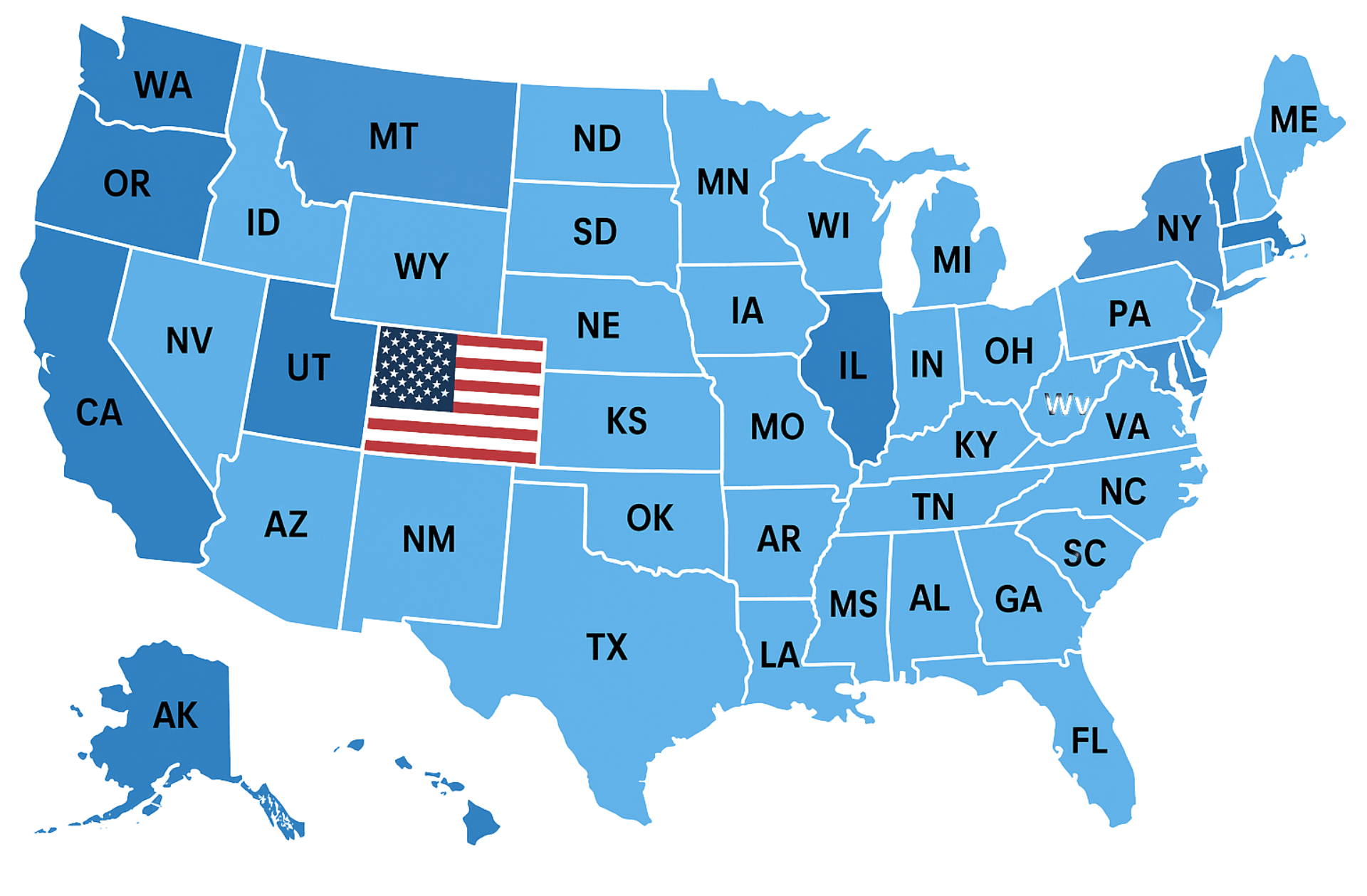
Insurance Companies We Work With
We work with every health plan in the United States, including Medicare, Medicaid, major commercial carriers like Aetna, Cigna, Humana, Blue Cross Blue Shield, UnitedHealthcare, as well as HMO, PPO, POS, state, and regional plans. Our team ensures seamless credentialing and contracting across all payers.
Save Time & Money with Our Medical Billing Service
Specialties We Serve
From primary care to mental health, urgent care to specialty practices, we support providers in nearly every field of medicine. Our services are tailored to the unique challenges of each specialty to help your practice thrive.
Family Medicine
Nurse Practitioners
Internal Medicine
Pediatrics
OB/GYN
Pain Medicine
Sleep Medicine
Cardiology
Dermatology
Endocrinology
Gastroenterology
Neurology
Podiatry
Pulmonology
Physical Therapy
Urgent Care
Psychiatry
Anesthesiology
Speech Therapy
Occupational Therapy
Otolaryngology (ENT)
Physical Medicine & Rehab
Geriatrics
Allergy & Immunology
Mental Health Therapists
Nephrology
Ambulatory Surgery Center
Wound Care
Addiction Medicine
Infectious Disease
Trusted by Healthcare Providers Nationwide











Very attentive and efficient
Always available to explain things or answer questions or concerns












We would love to hear from you.
Contact Us
Have a question or want to learn more about our services? Fill out the form below and our team will get back to you within 24 hours.
We serve all 50 states.