The Ultimate Guide to Credentialing for Mental Health Providers
In the vital field of mental health, **credentialing** is the bedrock of trust and professionalism. It ensures that providers—psychologists, counselors, therapists, and social workers—meet the rigorous qualifications required to deliver quality care. With the demand for mental health services at an all-time high, navigating the intricate and often overwhelming credentialing process is a critical challenge.
This guide explores the top credentialing services available, highlighting their features and benefits, and explains how partnering with an expert service can liberate you to focus on what truly matters: helping your clients thrive.
Why Credentialing is Non-Negotiable for Your Practice
Credentialing is far more than a bureaucratic hurdle; it's a foundational process that validates your expertise and unlocks your practice's potential. It serves several essential purposes:
Establishes Patient Trust and Safety
First and foremost, credentialing protects patients. By verifying your education, licensure, and work history, it assures clients they are receiving care from a qualified, vetted professional. This is the cornerstone of a therapeutic alliance.
Unlocks Access to Insurance Networks
To grow your practice, you need to be in-network with insurance payers. Credentialing is the only way to achieve this, expanding your potential client base exponentially and enabling you to accept a wider range of payment options. This is crucial whether you're wondering who can bill Medicare or how to credential with BCBS.
Enhances Professional Reputation and Credibility
Being credentialed signals to clients, colleagues, and healthcare systems that you adhere to the highest professional standards. It solidifies your reputation and opens doors for referrals and collaborative opportunities.
Where a Provider's Time is Spent in Credentialing
An estimated breakdown of the administrative burden on providers.
How to Choose the Best Credentialing Service
When searching for a credentialing partner, mental health providers should evaluate services based on several key factors:
Efficiency and Speed
The right service will dramatically streamline the process, minimizing administrative tasks and reducing turnaround times. This allows you to start seeing insured clients and generating revenue sooner. The cost of credentialing is often offset by the speed to reimbursement.
Expertise in Mental Health
Mental health credentialing has unique requirements that differ from other medical fields. A specialized service understands the nuances of payers like Aetna, Medicare, and Cigna for behavioral health, ensuring accuracy and avoiding common pitfalls. This is why our services for mental health providers are so critical.
Accreditation and Compliance
Choose a service that adheres to industry standards and is recognized for its best practices. This demonstrates a commitment to quality and compliance, protecting you and your practice. A deep understanding of platforms like CAQH is a must.
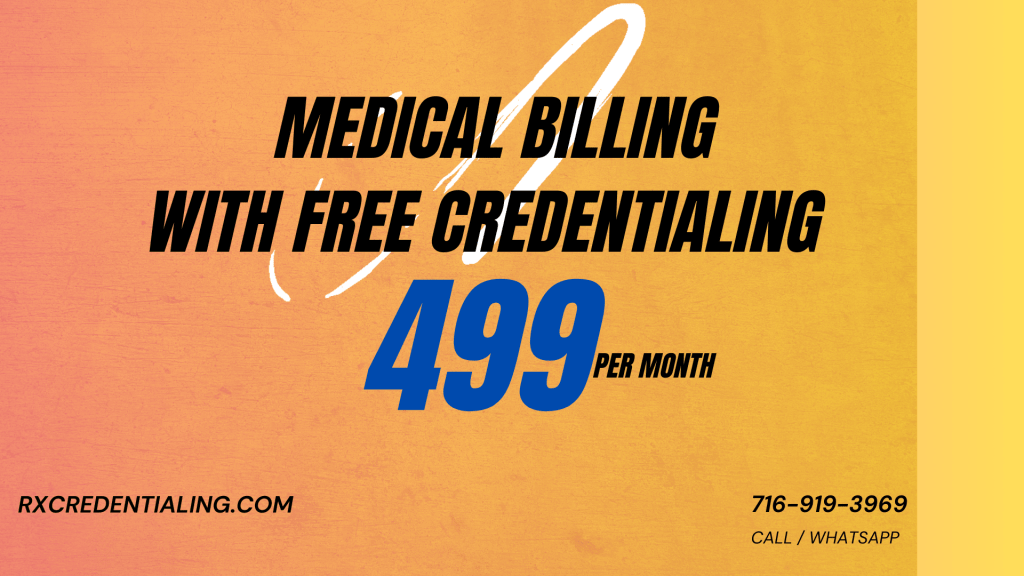
Why RxCredentialing is the Premier Choice for Mental Health Providers
RxCredentialing stands out as the top choice for professionals seeking efficient, reliable, and specialized credentialing services. Here’s why we are the preferred partner for therapists, counselors, and psychologists nationwide.
A Fully Streamlined Process
Our user-friendly platform and optimized workflows simplify the entire application and verification process, drastically reducing your administrative burden and saving you invaluable time.
Unmatched Mental Health Expertise
We specialize in mental health credentialing. Our experienced team is deeply versed in the specific requirements for various licenses (LCSW, LPC, PhD, PsyD) and payer policies, ensuring flawless and efficient processing.
Extensive Payer Enrollment Network
We have cultivated strong, established relationships with a vast network of insurance panels. This facilitates smoother, faster payer enrollment, allowing you to start accepting insurance reimbursements promptly.
Commitment to Compliance
We are dedicated to maintaining the highest standards. Our team stays constantly updated on the latest regulations and industry changes, ensuring your practice remains fully compliant with all legal and regulatory requirements.
Personalized, Dedicated Support
We provide dedicated customer support throughout the entire credentialing journey. Our knowledgeable team is always available to answer your questions and offer expert guidance, providing you with complete peace of mind.
Conclusion: Invest in Your Practice's Future
Choosing the right credentialing service is a critical business decision for any mental health provider. By partnering with a specialist like RxCredentialing, you offload the administrative complexities and ensure your practice is built on a compliant, profitable foundation. This allows you to dedicate your energy to your primary mission: delivering high-quality, life-changing care to your clients.
Frequently Asked Questions
The duration varies based on the payer, the completeness of your application, and the responsiveness of third-party verification sources. On average, it can take anywhere from 60 to 120 days. An expert service can often accelerate this timeline by preventing common errors and delays.
Absolutely. A key benefit of using a service like RxCredentialing is our ability to manage applications for multiple insurance panels simultaneously. We streamline the process, saving you hundreds of hours of redundant paperwork and follow-up.
While not required for payer reimbursement, many private pay providers still pursue credentialing to enhance their professional credibility. Furthermore, should you ever decide to accept insurance, the process will already be complete. For more details, read our guide on starting a private practice.
Compliance is crucial. It ensures you operate within legal boundaries, uphold ethical standards, and protect patient privacy according to HIPAA. It also involves attesting to your qualifications accurately to prevent fraud. Failure to comply can result in severe penalties and loss of licensure.
Our established relationships with payer networks give us direct lines of communication, which we leverage to expedite your application. We know precisely what each payer requires, how to present your information, and how to follow up effectively to ensure your enrollment is processed as quickly as possible.