Credentialing with UnitedHealthcare (UHC) is a pivotal step for healthcare providers aiming to serve a broader patient base and ensure timely reimbursements.
This guide delves into the intricacies of the UHC credentialing process, offering insights, resources, and best practices to navigate it efficiently.
Understanding UnitedHealthcare Credentialing
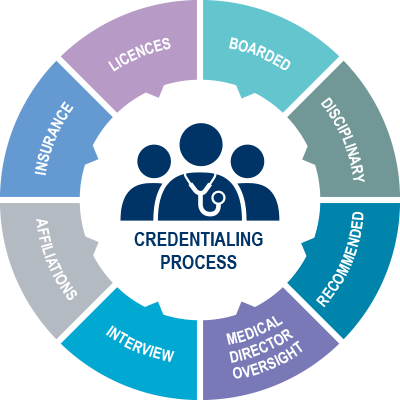
Credentialing is the process by which UHC verifies a provider’s qualifications, including education, licensure, and experience, to ensure they meet the organization’s standards for delivering care.
Why Credentialing Matters
-
Patient Trust: Credentialing assures patients that providers meet established standards.
-
Network Inclusion: Only credentialed providers can join UHC’s network, expanding patient reach.
-
Reimbursement Eligibility: Credentialed providers are eligible for timely reimbursements from UHC.
Step-by-Step Credentialing Process
1. Preparation
Before initiating the credentialing process, gather the following:
-
Tax Identification Number (TIN)
-
Educational and Training Certificates
-
Work History and References
2. CAQH ProView Registration
UHC utilizes the Council for Affordable Quality Healthcare (CAQH) ProView for credentialing. Ensure your profile is:
-
Complete: Fill out all sections accurately.
-
Up-to-Date: Regularly update any changes in your practice.
-
Authorized: Grant UHC access to your CAQH profile.
3. Submit Application via Onboard Pro
UHC’s Onboard Pro is the digital tool for credentialing:
-
Create an Account: Register using your One Healthcare ID.
-
Complete Application: Provide all necessary details and documents.
-
Track Progress: Monitor your application’s status in real-time.
4. Primary Source Verification
UHC will verify:
-
Education and Training
-
Licensure and Certifications
-
Malpractice History
-
Hospital Privileges
5. Credentialing Committee Review
A committee evaluates your application, considering
-
Qualifications
-
Practice History
-
Compliance with UHC Standards
6. Contracting
Upon approval:
-
Receive Contract: UHC will send a participation agreement.
-
Review and Sign: Ensure understanding of terms before signing.
-
Return Promptly: Expedite the process by returning the contract swiftly.
Recredentialing: Maintaining Active Status
UHC requires recredentialing every three years. To stay compliant:
-
Update CAQH Profile: Regularly attest and update your information.
-
Monitor Notifications: UHC will notify you when recredentialing is due.
-
Submit Timely: Avoid lapses in network participation by adhering to deadlines.
Common Challenges and Solutions
| Challenge | Solution |
|---|---|
| Incomplete Application | Double-check all sections before submission. |
| Outdated CAQH Information | Set reminders to update your profile quarterly. |
| Delayed Responses | Follow up with UHC if you haven’t received updates within expected timeframes. |
| Missing Documents | Maintain a checklist to ensure all required documents are submitted. |
Resources and Support
-
UHC Provider Portal: uhcprovider.com
-
CAQH ProView: proview.caqh.org
-
Credentialing FAQs: UHC Credentialing FAQs
-
Contact Support: Utilize the chat feature on the UHC Provider Portal for assistance.
Conclusion
Credentialing with UnitedHealthcare is a structured process designed to ensure that providers meet the organization’s standards for delivering quality care.
By understanding each step, preparing necessary documentation, and utilizing available resources, providers can navigate the credentialing process efficiently, leading to expanded patient reach and streamlined operations.
(FAQs)
How long does the UHC credentialing process take?
The process typically takes 45-60 days, but timelines can vary based on application completeness and verification processes.
Is CAQH registration mandatory for UHC credentialing?
Yes, UHC utilizes CAQH ProView for credentialing. Ensure your profile is complete and accessible to UHC.
Can I check the status of my application?
Yes, Onboard Pro allows real-time tracking of your credentialing application’s status.
What happens if my application is denied?
UHC will provide reasons for denial. You can address the issues and reapply after a specified period.
Do I need to recredential if I change practice locations?
Yes, significant changes like practice location may require recredentialing or updating your profile to reflect the changes.