Credentialing for Nurse Practitioners
Get in-network faster with Medicare, Medicaid, and commercial payers. We manage CAQH, applications, follow-ups, and contracting — so you can focus on patient care, not portals and paperwork.
- ✓ CAQH setup, updates & re-attestation
- ✓ Medicare & Medicaid enrollment support
- ✓ Commercial payer credentialing & contracting
- ✓ Proactive follow-ups + status updates
- ✓ Multi-state & multi-location support
- ✓ Clean submissions to reduce delays

Per payer application
What We Do
We provide comprehensive credentialing and payer enrollment services for healthcare providers and organizations, handling every step to ensure fast, accurate, and timely participation. From Medicare and Medicaid to commercial payers, we manage all administrative tasks so you can focus on patient care.
Medicare & Medicaid Enrollment
We handle the complete enrollment process for Medicare and Medicaid, from preparing and submitting applications to ensuring compliance, approvals, and timely participation so you can start seeing patients without delays..
Commercial Payer Credentialing
We manage credentialing for private insurance plans, including application submission, follow-ups, and verification, to help you join payer networks efficiently.
Contract Negotiationst
We review and negotiate contracts with payers to ensure favorable terms, clear reimbursement rates, and alignment with your practice goals.
Demographic & Ownership Updates
We handle updates to provider information, including practice location, tax ID, NPI, or ownership changes, keeping all payer records accurate and current.
Electronic Funds Transfer (EFT) Setup
We set up direct deposit with payers, ensuring timely reimbursement and reducing administrative delays for your practice.
Re-credentialing & Revalidation
We manage ongoing credentialing requirements, including provider re-credentialing and revalidation, so you stay compliant and in-network without disruption.
Who We Serve
We work with healthcare providers across all specialties and practice sizes. Whether you are a solo practitioner, a telehealth start-up, a multispecialty group, or a large healthcare system, we provide end-to-end credentialing and payer enrollment support.
Solo & Small Practices
Independent physicians, therapists, counselors, NPs, PAs, nutritionists & outpatient clinicians.
Group & Multi-Location Practices
Scaling practices needing rapid payer contracting for new clinicians or additional service sites.
Telehealth & Hybrid Care Models
National or multi-state virtual practices expanding payer coverage and participation.
How It Works
Our credentialing specialists take full ownership of your payer enrollment process. We complete and maintain your CAQH profile, submit all insurance applications, manage ongoing follow-ups with payers, negotiate contracts and fee schedules, and guide you through every step until your application is approved. With our end-to-end credentialing service, you avoid delays, reduce administrative burden, and get in-network faster.
CAQH Review & Optimization
We begin by reviewing and updating your CAQH profile to ensure all information, documents, and attestations are complete and current, setting a strong foundation for faster payer approvals.
Payer Enrollment Submission
Our team prepares and submits all required paper or electronic applications for your selected insurance panels, following each payer’s specific guidelines to avoid delays and rejections.
Proactive Follow-Ups
We communicate directly with payer representatives to track application status, provide any missing information, and keep the process moving, so nothing falls through the cracks..
Contracting Support & Final Approvals
Once approved, we review each contract with you, clarify reimbursement terms, and assist with next steps so you can confidently sign and start seeing in-network patients.
Benefits of Outsourcing
Credentialing for Nurse Practitioner
60-Day Medicare Approval
Average 60-day turnaround for Medicare vs. 6+ months when self-filing with pre-verified 855I forms.
CAQH ProView Management
Complete CAQH profile setup and quarterly attestations with error resolution.
Fee Schedule Optimization
Get optimal rates for NP-specific codes (99213-99215) before contract signing.
Specialty-Specific Filing
Tailored applications for Psych NPs, Pediatric NPs, and other specialties.
Telehealth Credentialing
Multi-state licensing and virtual care enrollment with major insurers.
Collaborative Agreement Compliance
Ensure supervisory documents meet state-specific requirements.
License Renewal Alerts
90/60/30-day alerts for state licenses, DEA, and NPI updates.
Denial Recovery
94% success rate fixing NP credentialing denials.
Revenue Cycle Integration
Seamless handoff to billing with proper NP provider numbers.
Have Other Questions? Get in Touch!
Our team is ready to guide you through every step of credentialing, contracting, and payer enrollment, making the process fast, simple, and stress-free.
The industry-standard timeline is 60 to 90 business days in most cases.
You get a dedicated credentialing manager who guides you and keeps you updated at every step.
No. You should wait for contract approvals before seeing patients.
We will need your state license, DEA, board certification, malpractice insurance, EIN Letter and a voided check to begin with the process.
We charge $140 per commercial application and $199 per government payer application. We do not charge any fee for closed panels.
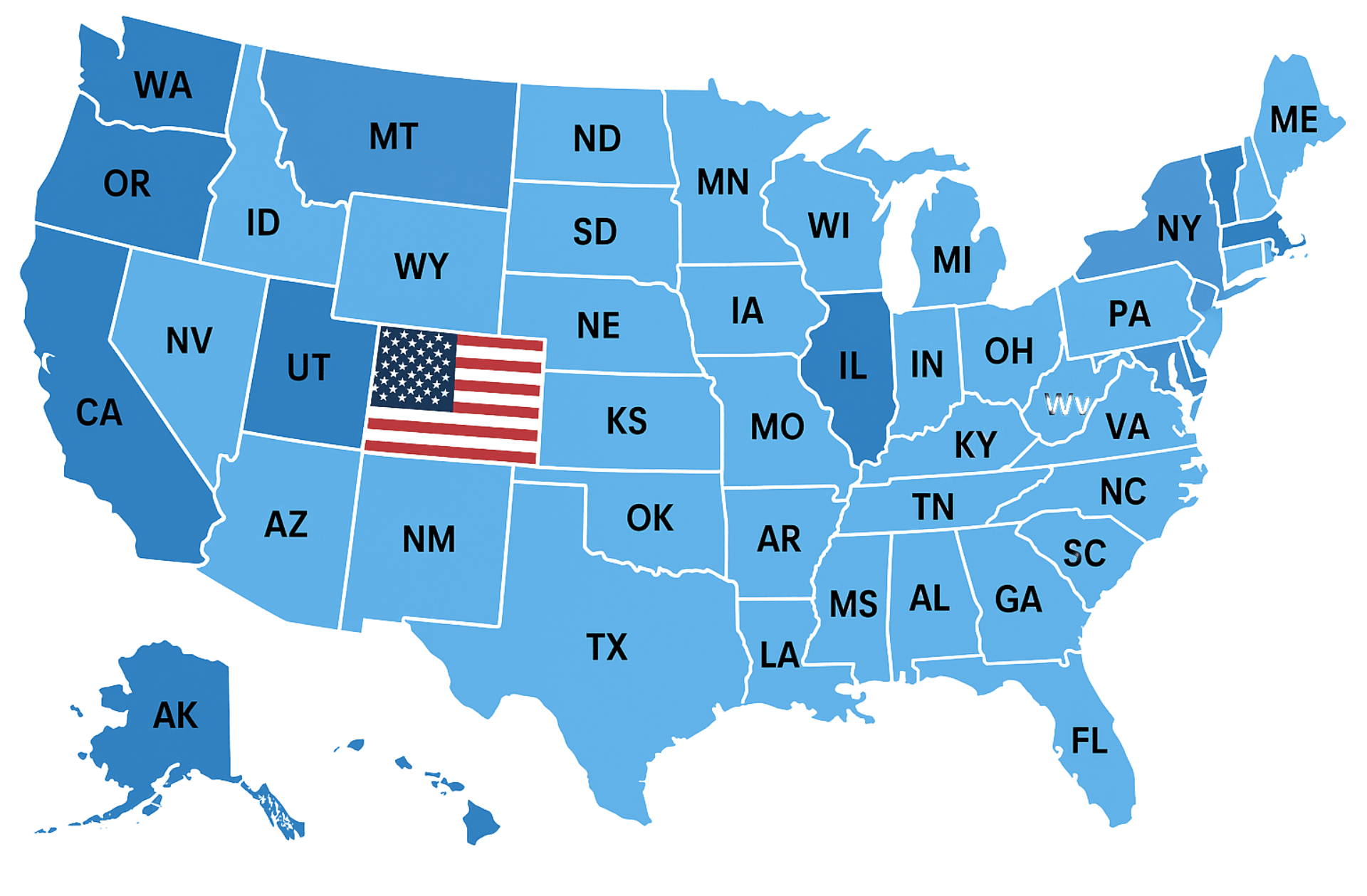
Insurance Companies We Work With
We work with every health plan in the United States, including Medicare, Medicaid, major commercial carriers like Aetna, Cigna, Humana, Blue Cross Blue Shield, UnitedHealthcare, as well as HMO, PPO, POS, state, and regional plans. Our team ensures seamless credentialing and contracting across all payers.
Trusted by Healthcare Providers Nationwide












Very attentive and efficient
Always available to explain things or answer questions or concerns












We would love to hear from you.
Contact Us
Have a question or want to learn more about our services? Fill out the form below and our team will get back to you within 24 hours.
We serve all 50 states.