Verification of Benefits Services for Healthcare Providers
Fast, accurate, and proactive VOB support that prevents denials and keeps your revenue flowing. Eliminate surprises, reduce denials, and strengthen your entire revenue cycle with precise, front-end benefit verification.
- Eligibility Confirmed 24 Hours Before Every Visit
- Coverage Verified: Primary & Secondary Identified
- Copay for the Visit Determined
- Provider Network Status Verified
- Authorization & Referral Requirements Checked
- Deductibles & Coinsurance Confirmed
What Our VOB Specialists Do
Know every patient’s coverage before they walk in.
Our VOB specialists verify eligibility and benefits across all active insurance plans a patient carries. We confirm network status, copays, deductibles, coinsurance, out-of-pocket limits, and coordination of benefits clearly identifying which plan is primary, secondary, or tertiary so your team knows exactly what to collect and what to expect from payers. With clean, upfront verification, you prevent denials, reduce billing delays, and ensure every claim is set up to get paid on the first submission.
Eligibility Verification
We confirm each patient’s insurance eligibility 24 hours before their visit, ensuring they have active coverage at the time of service.
Coverage of All Insurance Plans
Our specialists verify benefits across all active plans a patient carries, including primary, secondary, and tertiary coverage.
Copay & Patient Responsibility
We confirm the exact copay, coinsurance, and any outstanding deductible for the visit, so your team can collect the correct amount upfront.
Network Status Verification
We confirm whether your practice is in-network for the patient’s insurance plans, preventing claim denials and out-of-network billing surprises.
Authorization & Referral Checks
Our team identifies if prior authorizations or referrals are required for the scheduled service, helping you avoid denied or delayed claims.
Coordination of Benefits
We clearly determine which insurance acts as primary, secondary, or tertiary, making sure all claims are processed in the correct order.
Service Coverage Confirmation
We verify whether the specific service the provider will perform is covered under the patient’s insurance plan, preventing denied claims and unexpected patient bills.
Benefit Limit Confirmation
We verify coverage limits, visit allowances, and service caps to prevent rejected claims or unexpected patient bills.
How Our VOB Services Help Private Practices
Knowing patient insurance coverage, network status, and financial responsibility upfront helps practices avoid denied claims, surprise balances, and billing delays.
Reduce Denials & Delays
With complete benefit verification upfront, your practice avoids denied claims and billing delays, keeping revenue flowing smoothly.
Improve Point-of-Service Collections
Knowing copays, coinsurance, and outstanding deductibles in advance allows your staff to collect accurately at the time of visit.
Eliminate Surprise Patient Balances
Patients are informed about their financial responsibility ahead of time, reducing confusion and improving satisfaction.
Ensure Network Compliance
Confirming provider network status before visits helps avoid out-of-network issues and rejected claims.
Streamline Revenue Cycle
From eligibility to benefits coordination, VOB services simplify front-office operations and accelerate claim submissions.
Focus on Patient Care
By outsourcing verification, your team can spend more time delivering care instead of chasing insurance details.
Getting Started With Our VOB Services
The onboarding process takes just 1–2 days. It begins with a discovery call, where we learn about your practice’s needs and gather relevant information. We then assign a dedicated VOB specialist for the agreed number of hours and set them up as a user in your EHR. Your specialist will immediately begin verifying patient coverage, copays, network status, and authorizations—giving your practice complete clarity before every visit.
Discovery Call
We discuss your practice’s needs and gather relevant information to tailor our VOB services.
Dedicated VOB Specialist Assigned
We assign a trained specialist exclusively to your practice for consistent, reliable support.
EHR Setup
Your team sets up the VOB specialist as a user in your EHR for secure access to patient schedules and records.
Benefit Verification Begins
Your specialist starts verifying patient coverage, copays, network status, and authorizations.
Complete Pre-Visit Clarity
Your practice receives accurate, upfront information, reducing surprises and improving revenue cycle efficiency.
Specialties We Serve
From primary care to mental health, urgent care to specialty practices, we support providers in nearly every field of medicine. Our services are tailored to the unique challenges of each specialty to help your practice thrive.
Family Medicine
Nurse Practitioners
Internal Medicine
Pediatrics
OB/GYN
Pain Medicine
Sleep Medicine
Cardiology
Dermatology
Endocrinology
Gastroenterology
Neurology
Podiatry
Pulmonology
Physical Therapy
Urgent Care
Psychiatry
Anesthesiology
Speech Therapy
Occupational Therapy
Otolaryngology (ENT)
Physical Medicine & Rehab
Geriatrics
Allergy & Immunology
Mental Health Therapists
Nephrology
Ambulatory Surgery Center
Wound Care
Addiction Medicine
Infectious Disease
Have Other Questions? Get in Touch
Our team is here to help you understand how our VOB services can help you reduce denials and support consistant cashflows. We make the entire experience simple, transparent, and stress-free..
VOB confirms patient coverage, copays, deductibles, and authorizations before the visit.
Onboarding takes just 1–2 days, starting with a discovery call.
Yes. All our VOB specialists follow HIPAA-compliant workflows to keep patient data safe.
Upfront verification ensures accurate collections, fewer denials, and faster claim reimbursements.
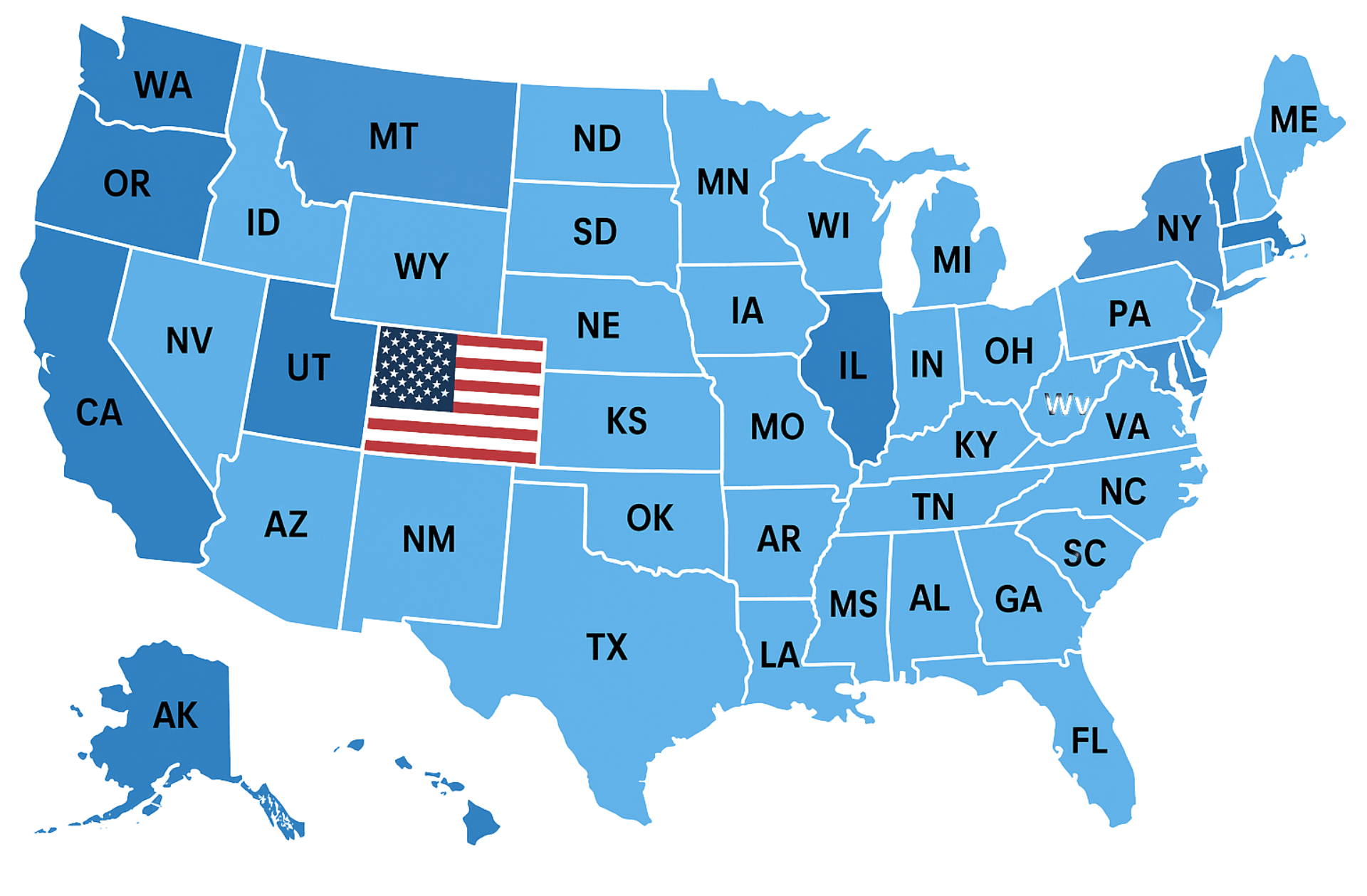
Trusted by Healthcare Providers Nationwide












Very attentive and efficient
Always available to explain things or answer questions or concerns












We would love to hear from you.
Contact Us
Have a question or want to learn more about our services? Fill out the form below and our team will get back to you within 24 hours.
We serve all 50 states.