Helping Medical Practices Optimize Revenue
Insurance Credentialing Service for Physicians
- Medicare and Medicaid Enrollments
- CAQH Registration and Attestations
- Commercial Insurance Credentialing
- Contract Negotiations
- Demographic updates
- Re-Credentialing Services
- EFT Setups
- Hospital Admitting Privileges
- IPA Enrollments
- Directory Verifications
zero
upfront fee
Medical Credentialing Services
starting from
$ 140
PER application
Seamless Service
Premium
Medical Credentialing Service
Unlock Seamless Billing with Our Premium Medical Credentialing Service
Are you tired of navigating the maze of insurance credentialing for your medical practice?
Look no further! Our expert team specializes in credentialing physicians, physician assistants, nurse practitioners, physical therapists, and social workers with top-tier insurance companies at unbeatable rates.
Say goodbye to the hassle of paperwork and bureaucratic delays. Our streamlined process ensures quick and efficient credentialing, so you can focus on what truly matters – providing exceptional care to your patients.
With our comprehensive service, you’ll gain access to a network of the best payers in your area, allowing you to accept every patient with confidence.
No more missed opportunities or revenue losses – start billing insurance companies right away and maximize your practice’s potential.
Don’t let credentialing woes hold you back. Partner with us today and experience the difference of seamless billing and increased efficiency for your medical practice.
Trust in our expertise to elevate your practice to new heights!
SERVICE FEATURES
CREDENTIALING SERVICES
- Pay As Your Go
- No Upfront Fee
- No Approval No Fee Policy
- Bi-weekly Status Reports
- Proper Step Wise Application Process
- Payer Evaluation To Choose the Best Payers In Your Area
- Pay As Low As USD 399 Per Provider Per Month
- No Hidden Fee Or Extra Charges As Others Do
- Professional Staff Knows Exactly What To Do
- We Review Each Contract and Negotiate If Applicable
- Free Consultation to Help You Navigate the Appropriate Entity Structure
- Provider credentialing Services for all 50 States and 100 Plus Specialties
our scope
More for you
Physician credentialing is important to build a patient network.
No matter what specialty and caliber you have, in order to gain a good patient volume you need to be listed on the insurance panels.
Healthcare insurances will only refer their patients to you if you are one of their participating or in-network medical provider.
You revenue cycle depends on physician credentialing.
Patients are the most basic need of a your medical practice so to make sure that you are not losing a single patient you should get into every insurance plan that is available in your area.
In simple words, it’s all about your cash-flows, if you have an existing medical practice or planning to start one, you should be well aware that all your plans run around cash-flows, which is dependent on proper provider enrollment process execution.
Right provider credentialing services enables you to accept more patients.
Provider credentialing with insurance payers is the first step to generate continues & healthy cash-flows.
Provider Credentialing ensures that you accept all the patients.
You will not have to say “NO” to any patient as you don’t accept that healthcare insurance they have.
In-network contracting helps you build strong brand.
Provider credentialing paves your way to payer network contracting, which means you will be get patients from other physicians from same network, this helps strengthen the relationship and build reputation with other providers & more patients.
Payer in-network contracting ensures more revenue for in-network providers Insurance credentialing has direct impact on your business plan.
If you will not get yourself or new hires credentialed in timely fashion, you will not be able to bill the insurance payers.
It may push you to plan cash arrangements from other resources.
While creating your medical practice business plan, always keep in mind the time it will take to get your in-network reimbursements for patients treated by newly credentialed providers.
Outsourcing physician credentialing process to right company can help you make best estimate.
Further you should also consider from what date newly hired medical providers can start seeing patients as if you will start billing for their patients on a future date, You need to know the cutoff date from where the payer can cover your past bills.
Commercial plan contracts do not have any retroactive billing provisions, so you will only be able to receive full reimbursement after your effective date.
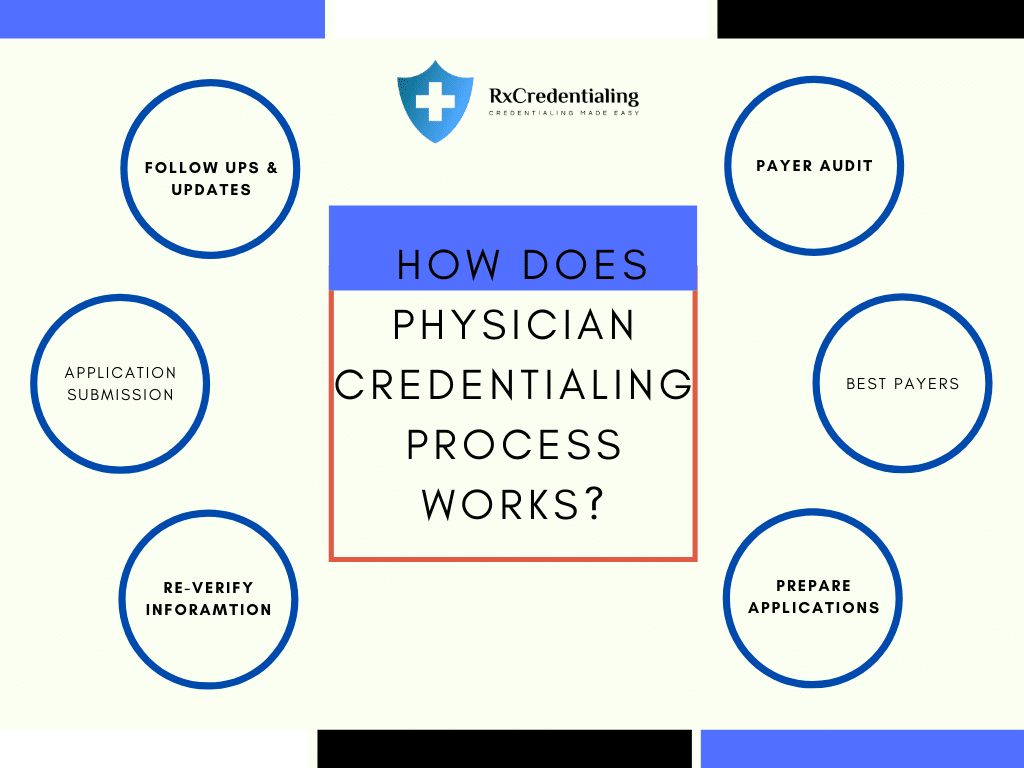
First Step:
We complete your CAHQ application and upload all the required documents.
Second Step:
We reach out to all the healthcare insurance carriers that you are planning to join and request application packets, complete the paperwork and submit back.
Third Step:
The third step to complete your physician credentialing process is to sign a contract with the medical insurance companies and accept terms and conditions.
Once we complete all above steps, Physician will become an in-network provider.
Physician will be able to receive reimbursements from each insurance payor.
We offer comprehensive provider credentialing service by analyzing the top payers in your area.
This enables you to improve your cashflow.
It is process of primary source verification for physician‘s education, experience and other related credentials.
The same concept is also known as insurance credentialing, medical credentialing and provider credentialing or enrollments.
The objective of medical insurance credentialing process is to make sure that all the information provided by medical provider in his or her physician credentialing application is correct.
This insurance credentialing process helps to minimize the risk of fraud.
It is to ensure highest level of patient care from qualified practitioners and improves quality assurance.
A primary source for your educational background could be the medical school you attended in order to earn your medical degree or certificate.
For work experience it could be your previous employer to verify expertise of healthcare providers. For licensure it will be your state medical board certification.
It also encompass verification or attestation of training and education through the American Medical Association or the Educational Commission for Foreign Medical Graduates if the medical provider got his medical education outside the United States.
Medical insurance payers can also verify Medicare sanction information from National Practitioner Data Bank on closed and settled claims history.
It can take 30 to 120 business days. It also varies payer to payer as some insurances may process your application within 15 days and some may take up to 6 months.
No doubt that medical credentialing is an important aspect for running a successful medical practice.
You can hire a provider credentialing specialist or outsource the process to right credentialing service provider company.
Our experience helps you save time and money. We Can Save Your Time by Avoiding Following Major Mistakes.
- Submitting credentialing applications with erroneous data.
- Submitting credentialing applications to wrong departments.
- Submitting multiple applications.
- Incorrect contracting or unable to understand the provider contract with insurance payers.
- Irregular follow ups.
- Provider enrollment with HMOs & PPOs without completing Medicare & Medicaid enrollment
- Signing an insurance contract without even reviewing it.
- Accepting the fee schedules from insurance companies as it is where it can be negotiated.
Choosing best credentialing services company for physicians can help you grow faster. It saves lot of time and effort you need to put to achieve physician credentialing goals.
The best company should always meet the deadlines. Delaying provider credentialing will not only effect your cash flow but over all operations as well.
The dedicated expert from best credentialing service company should evaluate and suggest top medical insurance payers in your area.
Segmenting and prioritizing medical insurance credentialing application process is key to success.
Medical insurance credentialing company should handle all re-validation or rec-credentialing tasks.
The company should be able to provide bi-weekly application status reports and charge competitive fee for insurance credentialing services.
COMMON QUESTIONS
The standard time frame for physician credentialing application process is 30-120 business days, Some insurances even take more than 120 days and some process applications within 45 days.
Your dedicated account manager will help you evaluate right payers according to your specialty and location. We help you negotiation contracts in best possible way. Transparent and timely client communication is main focus of our medical credentialing service. We send bi-weekly application status updates.
In general and on average, expect to pay $250-$399 per provider per payer for physician credentialing services.
No, you will have to wait until your medical provider credentialing and contracting application gets approved.
To complete medical provider credentialing process you should have following documents.
- State License
- Malpractice insurance
- DEA certificate
- Resume
- Board certificate
- IRS letter (EIN letter)
- Business Voided Check
- General Liability insurance
- Educational and Professional history of medical provider
- Article of Incorporation in case of business
We have also given detailed list checklist section. Do scroll down to check that.
Yes & No.
It depends on your specialty, patient volume and state you are practicing in but it is always recommended to complete your Medicare provider enrollment process before applying for other insurances.
It depends on multiple factors such as your Specialty, The state you are practicing in and the Insurances you are applying for.
We can help you get your individual or business NPI within 24 hours for FREE of Cost.
Yes, you will either get an approval letter via mail or an email from medical insurance payer on approval of your physician credentialing application.
Our Medical Credentialing Services include
- Provider and Practice NPI Registration
- CAQH Registration
- Medicare Provider Enrollment
- Medicaid Provider Enrollment
- Provider Credentialing with HMOs & PPOs
- Direct Deposit Setups- Medicare EFT
Physician Credentialing Checklist
Once you are ready to signup for insurance credentialing service , keep your documents ready related to following areas.
Physician information
Provider Name
NPI
Specialty
SSN
DOB
Provider Birth Country & State
Contact Number
Home Address
CAQH User Name & Password
NPPES User Name & Password
Office Hours
Practice information
Practice Name
Tax ID
Practice NPI
Practice Specialty
Service location
Mailing Address
Practice Phone Number
Practice Fax No
Owner information
Ownership Percentage
Owner Name
Owner DOB
Owner SSN
Owner Home Address Owner Cell
Owner NPPES User Name & Password
Owner Birth Country & State
WE OFFER INSURANCE CREDENTIALING SERVICE FOR
- Clinics
- House calls
- Private practices
- Telemedicine & Telehealth Startups
- Surgery centers credentialing
- Hospital Privileges
- IPA Affiliations
- Hospitals credentialing
MEDICAL INSURANCES WE COVER
- Medicare & Medicaid
- Tricare
- Aetna,
- Cigna,
- CBS,
- UHC,
- Humana
- All Managed Care & Regional Plans.







HOW DO WE SERVE
1-Contact
Simply explain what you want & leave your contact details. We will get back to you at our earliest.
2 - Information
After reviewing your query, we will get back to you as soon as possible to have clear idea regarding your requirements as well as we will help you to prepare specific documents required to complete the application.
2 - Submission
On your Go Ahead call, Our expert will update and submit the application to related departments.
Dedicated Manger will follow up with all verification resources as well as keep you posted regarding updates.
AFFORDABLE FEE
Get Following Covered for Only $ 140 per Application
- Life time support
- Get Credentialed with as many insurances companies as you want
- NPI registration & Maintenance
- CAQH Registration & Maintenance
- Medicare & Medicaid Enrollment
- Credentialing & Re-Credentialing with PPOs and HMOs.
- Contracting & Negotiations
- Direct Deposit Setups to avoid extra workload.
- Demographic Updates.
- Quarterly Directory Verification
WE LOVE TO HELP
Leave your question & contact. We will get back to you at earliest.