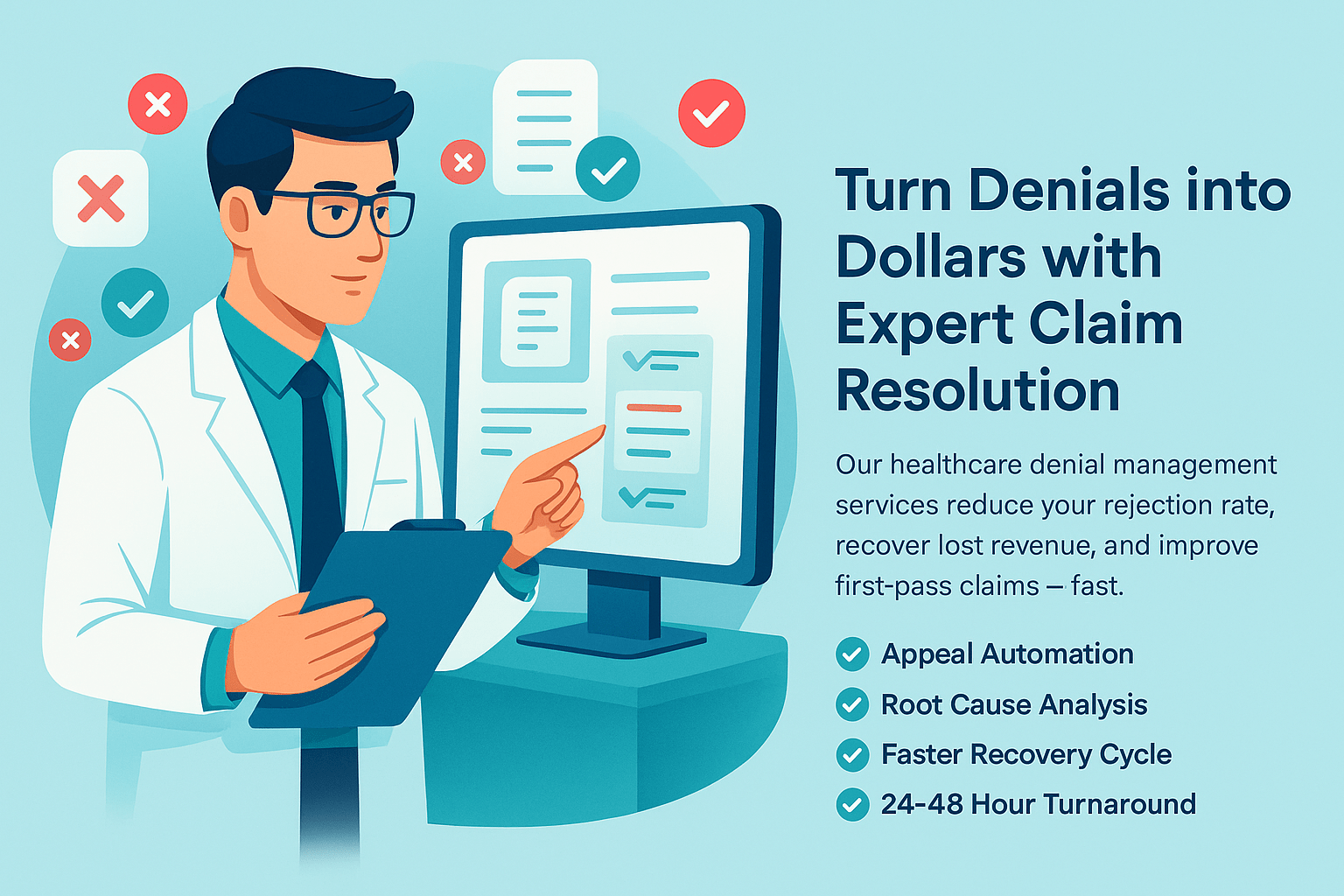
Healthcare Denial Management Services
Stop preventable denials from draining your cash flow. Our denial specialists identify root causes, correct claim issues, submit timely appeals, and build repeatable prevention workflows—so your clean-claim rate improves and AR days go down.
- ✓ Denial Root-Cause Analysis
- ✓ Corrected Resubmissions
- ✓ Appeal Writing & Tracking
- ✓ Timely Filing Protection
- ✓ Trend Reports & Prevention
- ✓ Faster AR Turnaround
What Sets Us Apart
Most denial work fails because it’s reactive—worked too late, without documentation context, and without a prevention plan. Our denial management approach is built around speed, accuracy, and repeatable fixes. We triage by payer deadlines, work denials based on root cause, and implement prevention controls so the same denial doesn’t come back next week. For payer policy reference, we align appeal and claim correction workflows with guidance used in Medicare fee-for-service administration through CMS MAC resources.
Denial Triage by Deadline & Dollar Value
We prioritize claims based on timely filing/appeal windows and reimbursement impact—so high-value denials don’t expire.
Root-Cause Fixes (Not Just Resubmits)
We identify why the denial happened (coding, auth, eligibility, documentation, edits) and apply targeted corrections.
Appeals with Supporting Evidence
We build clean appeal packets (notes, auth, medical necessity, payer refs) and track outcomes until resolution.
Full RCM Support Options
Need additional help? Pair denial work with AR recovery and medical billing to stabilize cash flow.
How It Works
We use a structured denial workflow: intake and categorization, correction and resubmission, appeals when needed, and prevention actions to reduce repeat denials. Our process is designed to integrate with your existing EHR and billing system so your operations stay uninterrupted and you can see progress clearly.
Step 1: Denial Intake & Categorization
We import denial data, categorize by payer/denial reason, and flag urgent items tied to timely filing or appeal limits.
Step 2: Investigation & Root-Cause Analysis
We review the claim, EOB/ERA, notes, and payer policy signals to identify the exact fix needed.
Step 3: Correct, Resubmit, or Appeal
We correct claims for clean resubmission, or write and submit appeals with supporting documentation when required.
Step 4: Track Outcomes & Prevent Repeat Denials
We monitor responses, escalate when necessary, and implement prevention steps (edits, training, auth checks) to reduce future denials.
Specialties we serve
Family Medicine
Nurse Practitioners
Internal Medicine
Pediatrics
OB/GYN
Pain Medicine
Sleep Medicine
Cardiology
Dermatology
Endocrinology
Gastroenterology
Neurology
Podiatry
Pulmonology
Physical Therapy
Urgent Care
Psychiatry
Anesthesiology
Speech Therapy
Occupational Therapy
Otolaryngology (ENT)
Physical Medicine & Rehab
Geriatrics
Allergy & Immunology
Mental Health Therapists
Nephrology
Ambulatory Surgery Center
Wound Care
Addiction Medicine
Infectious Disease
Have Other Questions? Get in Touch
Our team is here to help you understand every part of the billing process, from claim submission to reimbursement. Whether you need clarity on workflows, payer rules, or how our services fit your practice, we make the entire experience simple, transparent, and stress-free.
Our onboarding process is completed within 3–5 business days, provided all required information is supplied.
Yes — we work with nearly all popular platforms such as Tebra, OfficeAlly, eCW, Athena, DrChrono, AdvancedMD, SimplePractice, ICANotes, Optimantra, and more.
Our base plan starts at $499/month and includes free credentialing for solo practitioners. Standard billing plans are 3–5% of insurance collections.
Yes — we offer free credentialing, CAQH maintenance, and revalidation support for billing clients.
All PHI is handled in accordance with HIPAA requirements. Our team uses secure, encrypted systems for file storage, communication, and data access. Access to PHI is limited to authorized staff only, based on job responsibilities, and all activity is monitored.
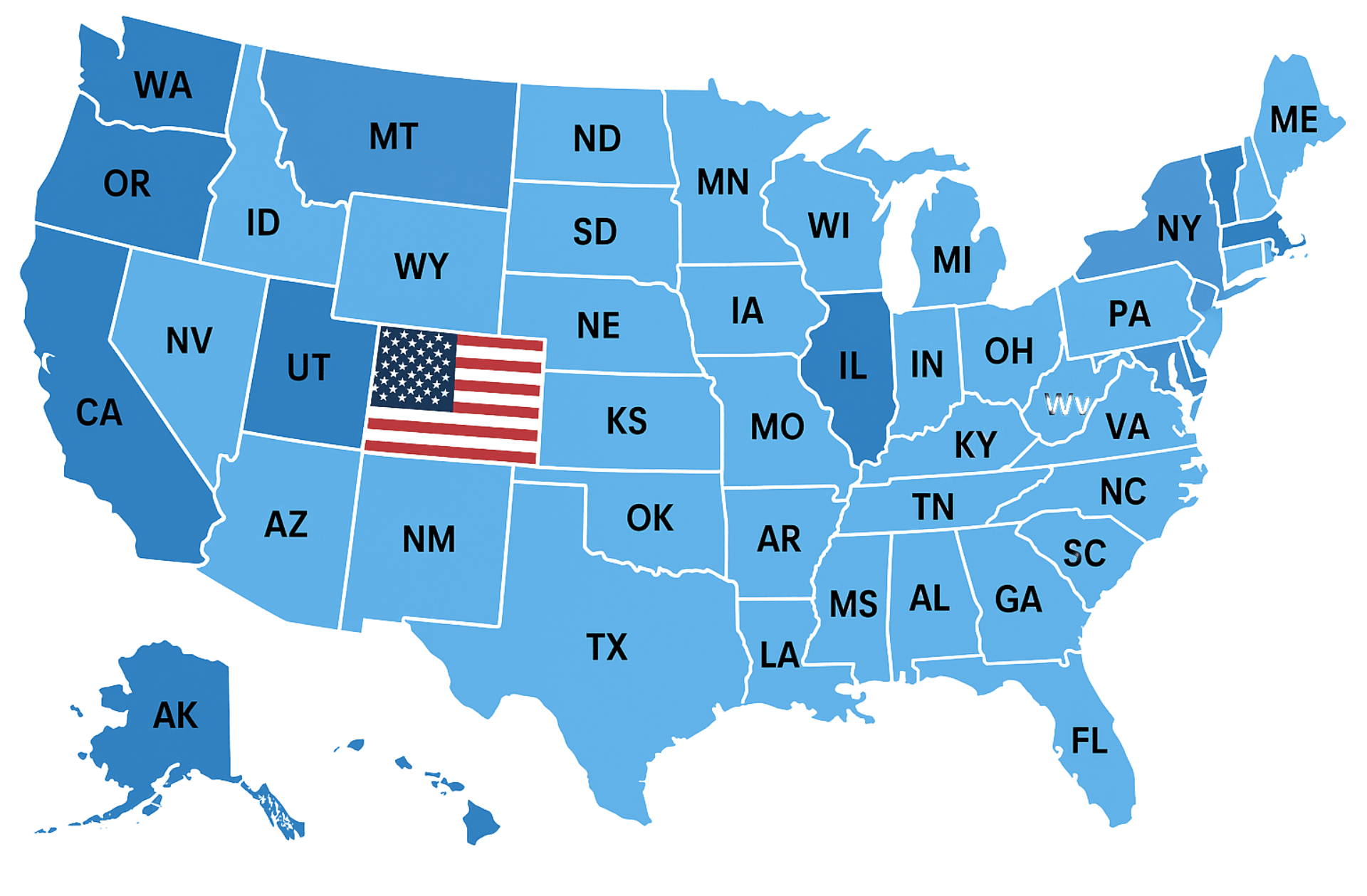
Insurance Companies We Work With
We work with every health plan in the United States, including Medicare, Medicaid, major commercial carriers like Aetna, Cigna, Humana, Blue Cross Blue Shield, UnitedHealthcare, as well as HMO, PPO, POS, state, and regional plans. Our team ensures seamless credentialing and contracting across all payers.
Trusted by Healthcare Providers Nationwide











Very attentive and efficient
Always available to explain things or answer questions or concerns












We would love to hear from you.
Contact Us
Have a question or want to learn more about our services? Fill out the form below and our team will get back to you within 24 hours.
We serve all 50 states.