Revenue Protection Series | Written by Adam Blake
The Bottom Line: What is TFL?
A Timely Filing Limit (TFL) is the strict deadline (measured in days) a payer allows for claim submission after a service is rendered. If a claim arrives even 24 hours late, it is denied as “untimely” (CO-29 denial code) with no appeal rights. For most small practices, this is the #1 cause of preventable revenue loss.
Timely filing is not a “suggestion”—it is a hard contractual rule. Unlike a coding denial which can be corrected, an untimely filing denial is usually permanent. For a small practice, missing these deadlines creates cash-flow instability and reputational damage.
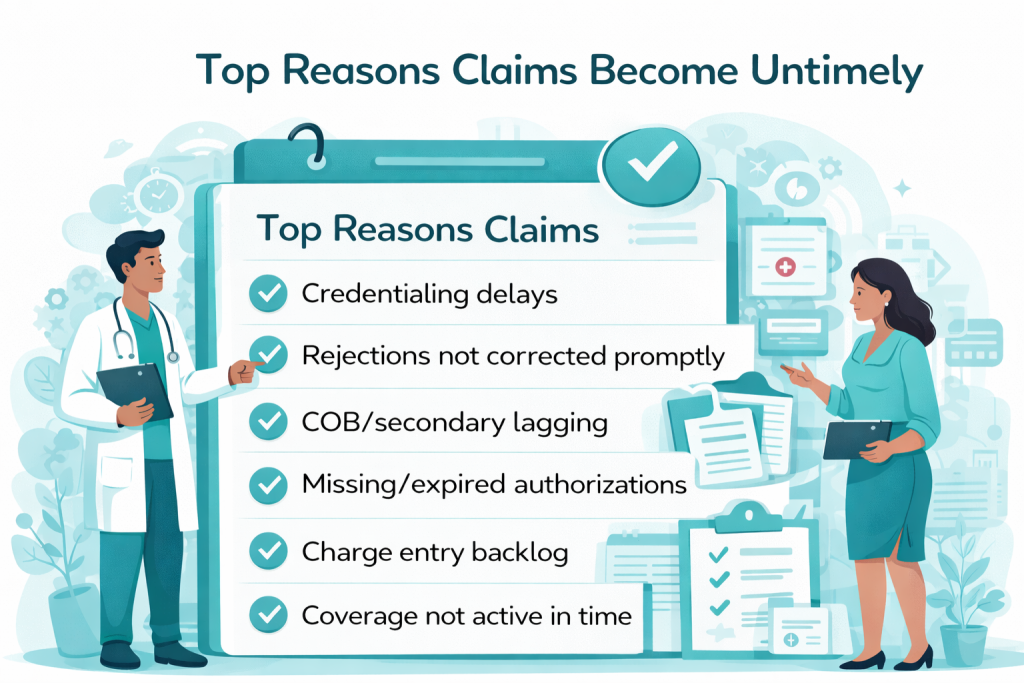
The biggest culprit? It’s rarely forgetfulness. It is usually credentialing delays or “pending” claims that sit unresolved until the clock runs out. If you are a new practice, ensure your NPI and taxonomy codes are active before seeing patients.
Master Payer Timelines (2026 Standards)
While contracts vary, most payers adhere to these standard windows. Warning: “Out-of-Network” claims often have much shorter windows (e.g., 90 days) than In-Network claims.
| Payer | Standard Limit (from DOS) | Exceptions |
|---|---|---|
| Medicare | 365 Days | Very strict. No extensions without “Good Cause” (e.g., administrative error by CMS). See CMS IOM Pub 100-04. |
| Medicaid | 90 to 365 Days | Varies wildly by state. HMO Medicaid plans (Managed Care) often have tighter 90-day limits. |
| Blue Cross (BCBS) | 90 to 180 Days | Some local plans allow 365 days, but many HMOs are strictly 90 days. Check your contract. |
| UnitedHealthcare | 90 Days | One of the tightest windows in the industry. Prioritize UHC claims weekly. |
| Aetna | 90 to 180 Days | Verify your specific fee schedule and contract. Late appeals are rarely accepted. |
The 3 Clocks You Must Watch
Most providers only watch the “Initial Claim” clock. This is a mistake. There are actually three separate timers running on every patient encounter. Missing any one of them results in a denial.
1. Initial Submission
Starts: Date of Service (Professional) or Discharge Date (Facility).
Ends: 90-365 days later.
Risk: High. If missed, 100% write-off.
2. Corrected Claims
Starts: Date of Rejection/Denial.
Ends: Often just 60 days.
Risk: You fix the error, but if you submit the correction too late, it’s denied.
3. Appeals
Starts: Date of Denial (Remittance Date).
Ends: 30-60 days.
Risk: Missing this window locks the denial in place permanently.
The Deep Dive: Proving You Filed on Time
If a payer claims they “never received” your claim, you must provide Proof of Timely Filing (POTF). This is where 90% of denial management efforts fail because providers submit the wrong evidence.
✅ Valid Proof (Acceptable)
- EDI 277CA Report: The digital acceptance receipt from the clearinghouse showing the claim was accepted by the payer’s gateway. This is the “Gold Standard.”
- Certified Mail Receipt: For paper claims, the green card signed by the payer’s mailroom.
- Portal Confirmation Number: A screen print of the payer’s direct portal submission screen with a “Received” status.
❌ Invalid Proof (Unacceptable)
- A screenshot of your EMR/EHR saying “Sent.”
- A regular postage receipt (doesn’t prove what was sent).
- A verbal reference number from a call center rep (often disputed).
Get Free Credentialing with Medical Billing
Stop losing revenue to the “Credentialing Gap.” Let us handle your entire cycle.
Prevention Playbook: The Weekly Routine
To avoid timely filing denials, you must move from “monthly” billing to “weekly” billing. Here is the workflow we use at RxCredentialing:
- Daily: Clear clearinghouse rejections. If a claim is rejected, the TFL clock is still ticking. It is not “received” until it is accepted.
- Weekly: Run an “Unbilled Encounters” report. Look for anything older than 14 days and fix the missing info (usually auths or credentialing issues).
- Monthly: Audit your “Pending” bucket. If a claim has been pending for 45 days with no response, call the payer immediately. Do not wait for 90 days.
If you are managing high-value claims like J3490 unclassified drugs, missing the deadline can cost thousands per claim. If your revenue cycle management team isn’t doing this, you are at risk.
Frequently Asked Questions
Does the timely filing limit start on the date of service?
For professional claims (CMS-1500), yes. For facility claims (UB-04), it typically starts on the discharge date (“Through” date).
What if I have secondary insurance?
The clock for secondary claims usually starts on the date of the Primary Payer’s EOB (remittance date), not the date of service. You typically have 90 days from the primary payment to bill the secondary.
Can I appeal a Timely Filing denial?
Only if you have valid proof (like a certified mail receipt or EDI report) or if the patient failed to provide insurance info on time (and you can prove it). Otherwise, TFL denials are very difficult to overturn.
How do credentialing delays affect TFL?
If you aren’t credentialed, you can’t bill. If your credentialing takes 120 days but the TFL is 90 days, you will lose that revenue. This is why understanding credentialing costs and timelines is critical.
About the Author: Adam Blake
Adam has helped hundreds of healthcare providers start, grow, and sustain medical practices with his 15 years of extensive experience in the field. He specializes in denial management, payer compliance, and revenue cycle optimization.