Navigating the complexities of medical billing can be challenging. This comprehensive guide breaks down everything you need to know about pricing, factors, and choosing the right partner.
For any healthcare practice, ensuring a steady and healthy revenue stream is paramount. The intricacies of medical billing, however, can often feel like a full-time job in itself. From complex coding to following up on denials, the process is both time-consuming and critical. This is why more and more providers are turning to professional medical billing services to streamline their revenue cycle management.
But how much do these services actually cost? The answer isn't a simple number. It depends on a variety of factors, including the services you need and the pricing model the company uses. In this guide, we will dive deep into the world of medical billing costs, helping you understand the options so you can make a financially sound and strategic decision for your practice.
What Exactly Do Medical Billing Services Include?
At its core, medical billing involves handling the administrative tasks related to the billing and collection process. While many practices may think of it as just submitting a claim, a full-service provider offers a much more robust suite of services. These can include:
- Credentialing and Enrollment: Getting providers properly credentialed with insurance payers is the first and most critical step. Without it, you cannot get paid. You can learn more about this process in our guide to credentialing with Aetna or our guide to credentialing with Blue Cross Blue Shield.
- Charge Entry and Coding: Accurate coding of diagnoses (CPT codes) and procedures is essential for proper reimbursement.
- Claim Submission: Submitting claims electronically to various insurance carriers, including commercial payers and government programs like Medicare (Medicare Credentialing).
- Denial Management and Appeals: Handling and appealing claims that have been denied or underpaid. Our denial management services are a great example of this.
- Accounts Receivable (AR) Follow-up: Proactively chasing unpaid claims to ensure maximum revenue recovery. This is a core part of our AR recovery services.
- Patient Billing and Support: Managing patient statements and inquiries, providing a seamless experience for your patients.
Key Factors Influencing Your Medical Billing Cost
When you get a quote from a medical billing company, it's a reflection of several variables that are unique to your practice. Understanding these will help you negotiate a fair price and avoid unexpected costs.
1. Practice Size and Claim Volume
The size of your practice is a major determinant. A small private practice with a single provider will have different needs and a different cost structure than a multi-specialty clinic with dozens of physicians. Higher claim volumes often lead to a lower percentage rate in a percentage-based model due to economies of scale.
Medical billing for small practices is typically more affordable and can offer more personalized service.
2. Medical Specialty
Certain medical specialties are more complex to bill for than others. For instance, billing for a simple primary care visit is straightforward. However, a specialty like cardiology, orthopedics, or oncology involves a multitude of specific codes, modifiers, and complex procedures that require a higher level of expertise. For example, our oncology medical billing services are tailored to handle the unique challenges of that field.
3. Scope of Services
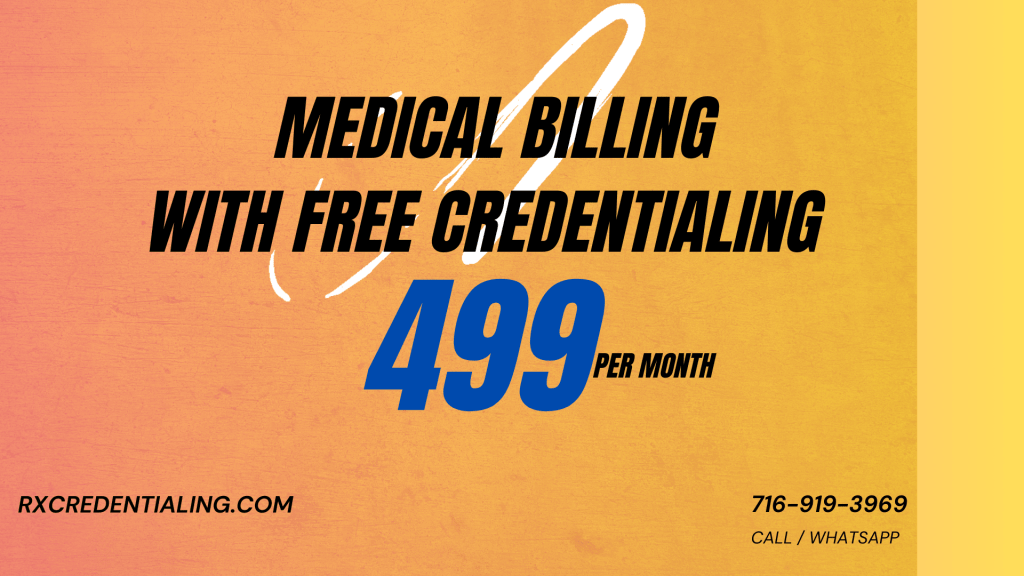
Do you need just claims submission, or do you require a full suite of physician billing services? The cost will increase if the service includes patient billing, credentialing, contract negotiations, or advanced reporting.
4. Geographic Location
While the rise of remote work has leveled the playing field, a provider's location can still influence cost. Services in areas with a higher cost of living may have slightly higher prices. However, a great service like Rxcredentialing can serve providers nationwide, offering competitive rates no matter where you are.
5. Technology & EHR Integration
A provider's technology stack is a significant factor. Services that offer seamless integration with your existing Electronic Health Record (EHR) system can be invaluable. Some services may charge extra for this integration or for access to their proprietary software. Learn more about the role of EHR systems in reducing billing errors.
A Detailed Look at Common Pricing Models
Understanding the different ways a medical billing company can charge you is key to budgeting effectively. Here are the most common pricing structures you will encounter.
Medical Billing Pricing Models Comparison
| Model | How it Works | Pros | Cons |
|---|---|---|---|
| Percentage-Based | Charges a percentage (typically 4-10%) of the total collected revenue. | Aligns incentives, no fee if no collections, scalable with practice growth. | Can be expensive for high-value practices, cost can fluctuate. |
| Flat Fee per Claim | A fixed rate per claim submitted (e.g., $5-$10 per claim). | Predictable costs, great for high-value claims, simple to budget. | May not be cost-effective for low-value claims, volume doesn't lower price. |
| Hourly Rate | Billing for time spent on tasks (e.g., $25-$45 per hour). | Best for specialized or short-term projects, full control over spending. | Can be unpredictable, requires close monitoring, less common for full RCM. |
| Hybrid Models | Custom combination of the above models to fit specific needs. | Maximum flexibility, tailored to practice's unique situation. | More complex to manage, requires a custom agreement. |
For a more in-depth look at all the factors, check out our article on how much do medical billing services cost?.
The Rxcredentialing Process: Getting Started
Before any billing can begin, your providers must be properly enrolled with insurance payers. At Rxcredentialing, we make this process as transparent and efficient as possible. Here is a simplified look at the steps we take to get you started:
1. Initial Consultation
We start with a free consultation to understand your practice's unique needs and goals. We'll discuss your specialty (e.g., anesthesia, OB/GYN), patient volume, and current challenges. This is where we lay the groundwork for a successful partnership.
2. Provider Enrollment
We handle the entire provider enrollment process, including CAQH credentialing, ensuring all paperwork is accurate and submitted in a timely manner. This minimizes delays and gets you on the path to receiving payments faster. We also assist with specialized needs like credentialing for nurse practitioners.
3. Seamless Onboarding
Our team will work with you to integrate our systems with your existing practice management software, ensuring a smooth transition. We provide comprehensive training and support, so your staff is comfortable with the new workflow.
4. Ongoing Management
Once everything is set up, our team takes over the daily billing tasks, providing you with real-time reporting and constant communication. This frees your team to focus entirely on patient care, knowing your finances are in expert hands.
Expertise, Authority, and Trust: Why It Matters
In the healthcare industry, there is no room for error. Your medical billing partner should not only be skilled but also knowledgeable about the latest regulations and compliance standards. This is where adherence to CMS guidelines and a deep understanding of the American Medical Association's CPT codes become critical. By choosing a partner with a proven track record, you are safeguarding your practice's financial health and reputation.
Choosing a partner is just as important as knowing the costs. Take a look at our guide on hiring an insurance credentialing service to learn more.
The Path to Financial Health for Your Practice
Choosing the right medical billing service is one of the most impactful decisions you can make for your practice. It's an investment that pays for itself by maximizing collections, reducing administrative overhead, and ensuring compliance. While cost is a major factor, remember to consider the provider's expertise, technology, and transparency. A great partner, like Rxcredentialing, offers more than just a service—they offer peace of mind.
Ready to learn more about how we can help your practice thrive? Contact us today for a personalized quote and see the Rxcredentialing difference.
Frequently Asked Questions (FAQs)
Click on a question to reveal the answer.
Outsourcing medical billing services allows healthcare professionals to focus on patient care, streamline revenue cycle management, reduce administrative burdens, and improve cash flow. It's an essential strategy for modern practices.
The implementation timeline can vary depending on the complexity of your practice and the chosen service provider. It may take a few weeks to set up the necessary systems, integrate software, and train staff. A streamlined process is key for a fast transition.
Yes, many medical billing service providers offer customizable solutions. It's best to discuss your specific needs—such as for specialized fields like gastroenterology or physical therapy—with a provider to tailor a solution that fits your unique requirements.
To avoid hidden costs, it's crucial to thoroughly review the service agreement and contract terms. Ask about additional fees for setup, software access, reporting, or denial management. A transparent provider will be upfront about all potential charges.
When choosing a provider, prioritize one that is HIPAA-compliant and follows strict security protocols. Look for features like data encryption, secure servers, and proper access controls to ensure patient information is protected. Protecting patient data is a top priority for all reputable billing services.
A percentage-based model charges a percentage of the total revenue collected, aligning the service's success with your practice's. A flat-fee model charges a fixed amount per claim or per month, which offers predictability but might be less cost-effective for practices with high claim values.