Criteria for Billing Chronic Care Management Services
So, you’re wondering how to bill for chronic care management services? Well, it’s essential to understand the key factors determining your eligibility to bill. It starts with the patient’s condition.
They should have at least two chronic conditions expected to last at least 12 months, or until the death of the patient. These conditions must pose a significant risk to their life, causing acute exacerbation or functional decline.
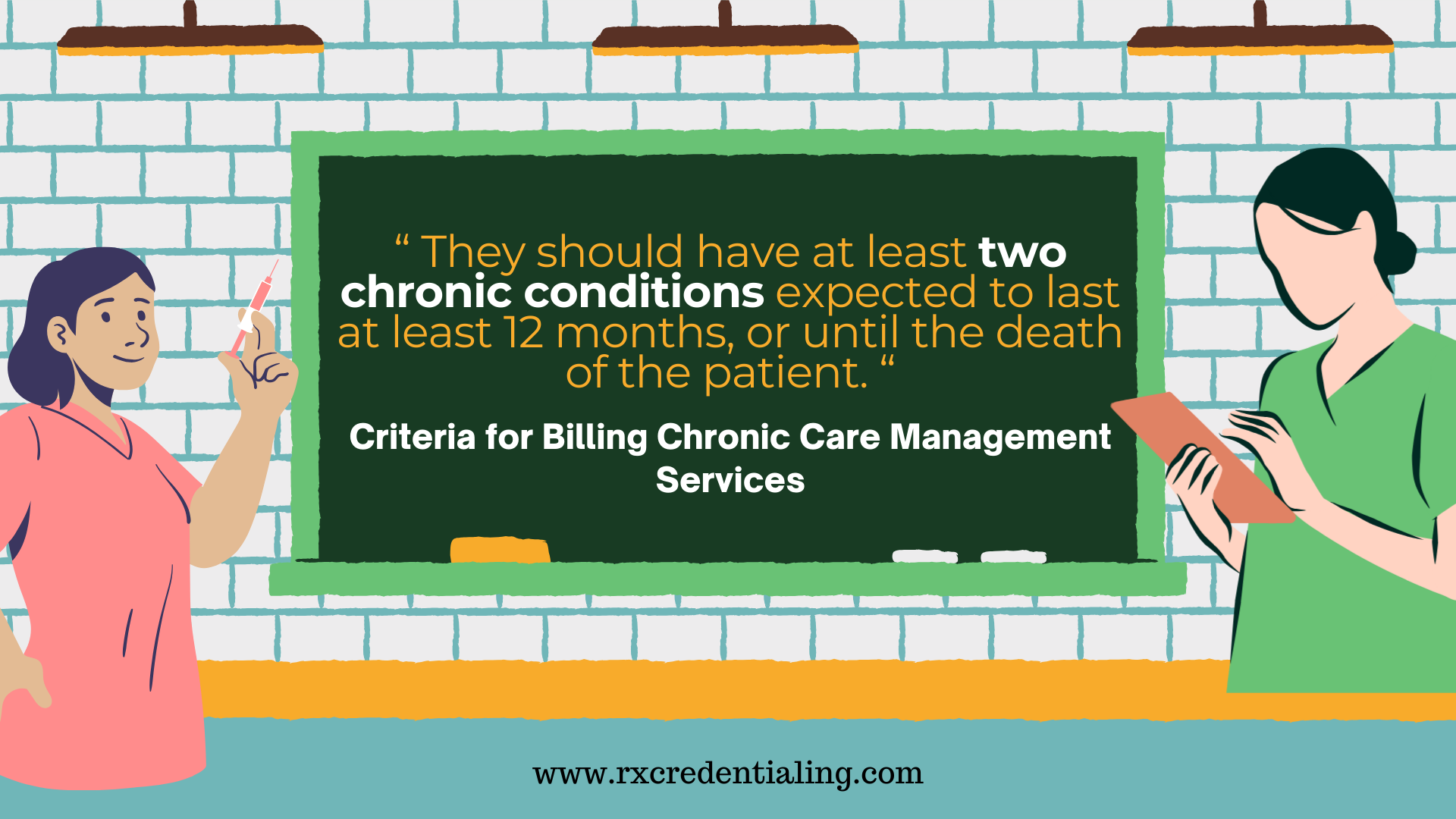
These conditions include, but are not limited to, diabetes, hypertension, cardiovascular disease, and cancer. A comprehensive care plan tailored towards managing these conditions forms the foundation for billing CCM services.
Next, make sure you have the patient’s consent. As a provider, you’ll need written consent before billing the patient or their insurance for chronic care management services.
While obtaining consent, it’s crucial to inform the patient about the service’s nature, potential risks, and benefits, including costs they might incur.
Another key criterion is the time spent on the service. To bill for CCM services, the clinician must spend at least 20 minutes per month on non-face-to-face care management activities for the patient.
These activities often involve coordinating care with other healthcare providers and setting up appointments for patients.
The last criterion to consider is proper documentation. As a provider, you are required to keep full documentation proving that the above conditions have been met.
This includes keeping copies of the patient’s care plan, their provided consent form, notes on time spent on CCM services, and any relevant communication with the patient and other healthcare providers.
Ensure that all documentation is readily accessible upon request to substantiate your claim.
Remember, understanding these key factors will not only make the billing process more straightforward but also ensure a smooth, compliant experience for both you and your patients. It’s a win-win situation!
Chronic Care Management (CCM) services are billable under Medicare Part B.
Care providers usually charge for these services under the Current Procedural Terminology (CPT) code 99490. To use this code, the patient must have at least two chronic conditions that are expected to persist at least 12 months, or until their death.
These conditions must put the patient at risk of death, acute exacerbation, decompensation, or functional decline.
To bill for CCM services under CPT 99490, a comprehensive care plan should be in place, established, implemented, revised, or monitored.
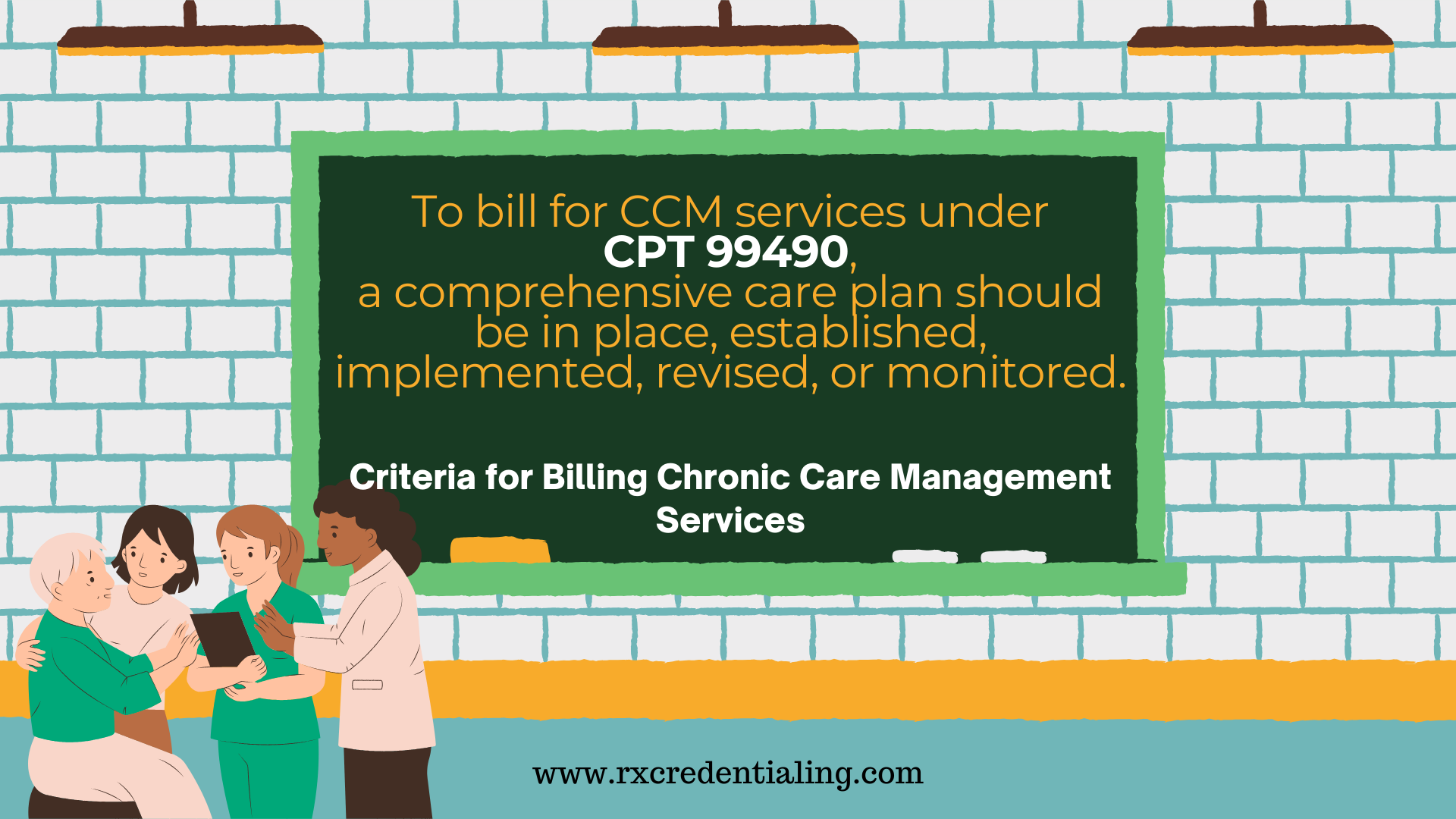
This plan should be accessible electronically 24/7 to all providers within the practice to ensure the continuity of care. And remember, only one practitioner can bill for CCM services per patient in a calendar month.
Additionally, Advance Consent must be obtained from the patient before these services can be billed.
This entails informing them about the availability of CCM services, what the services encompass, the applicable cost-sharing, the fact that only one clinician can furnish and be compensated for these services in a calendar period, plus right of the patient to suspend or revoke the services at any point of time, in writing.
Apart from CPT code 99490, there are additional codes that might be applicable depending on the situation, such as complex Chronic Care Management codes 99487 and 99489.
99487 is applicable if the patient requires at least 60 minutes of clinical staff time, and 99489 is an add-on code for every subsequent 30 minutes.
The billing process for Chronic Care Management services requires meticulous attention to detail to ensure each individual service is correctly calculated and billed.
Any inaccuracies can result in significant losses to practice revenue, so it’s crucial to get it right.
Key Aspects of Medicare’s Chronic Care Management Program
The Medicare Chronic Care Management program is an initiate designed to provide comprehensive support to Medicare beneficiaries suffering from multiple chronic illnesses.
This program focuses on ensuring coordinated care which can drastically improve the quality of life for patients, and lower healthcare costs by curtailing the need for additional treatments.
When it comes to billing for these services, there are a few key aspects to keep in mind.
Firstly, Chronic Care Management services offered under Medicare must be rendered by a physician, or other qualified healthcare professionals under the general supervision of a physician. This includes nurses, medical assistants and other healthcare providers.
Payments for CCM services under Medicare, are only made if the service meets specific requirements and is billed using the appropriate codes.
Reimbursements for Chronic Care Management services are typically received monthly, and the amount billed for depends on the complexity of the patient’s care needs.
For simple CCM services, Medicare has established codes such as 99490. For more complex cases, codes such as 99487 or 99489 can be used, where extra time and coordination are required.
Healthcare providers must note that these codes should be used appropriately to reflect the level of care provided and avoid over billing or under billing.
A last, but equally important aspect of the Medicare Chronic Care Management program, is the consent requirement.
Understanding these key aspects of the Medicare Chronic Care Management program is not only essential for appropriate billing, but can also help healthcare providers ensure they are providing the best possible care to their patients.
Patient Engagement: A Critical Component in Chronic Care Management Billing
Imagine yourself in your patient’s shoes. How can you ensure they truly understand the nature of their health issues, the reasoning for their management plan, and the costs associated with their care? The answer lies in patient engagement.
In maintaining a successful chronic care management billing process, your role extends beyond healthcare provider; you also become an educator.
This means it’s your responsibility to effectively communicate the reasoning behind your patient’s care plan, the possible costs they will incur, and the potential impact on their overall health.
Your patients, faced with a chronic illness, need and deserve to know how their care will be managed and what billing process is connected with it. So, don’t be afraid of those questions.
Be prepared to answer them with accuracy and ensure all aspects of their health care are transparent, especially when it comes to billing. This ties back to the importance of patient engagement.
A well-informed patient is more likely to be engaged in their healthcare journey.
Providing detailed information and actively addressing their concerns can greatly decrease the probability of misunderstandings regarding billing procedures or disappointment with unexpected charges.
As a medical provider, you can have direct influence on patient satisfaction and trust through proactive communication and transparency. This can also contribute to a smoother billing process, with prompt and conscientious payment of dues.
Remember, your commitment to patient engagement fosters an environment of trust, understanding, and efficiency – all crucial in optimizing your chronic care management billing practice.
Taking Advantage of Telehealth in Chronic Care Management Billing
In a swiftly evolving healthcare landscape, telehealth has surged to the forefront as a critical tool for medical professionals. The vast reach of digital technology can help your practice optimize the billing process for chronic care management (CCM) services.
For starters, telehealth services enable your team to provide CCM even for patients situated at a distance. You have the opportunity to fine-tune your billing strategies by capitalizing on this technological boom. Bear in mind, Medicare offers reimbursement for telehealth services.
Consequently, you should understand how to bill these components correctly.
Using telehealth technology, clinicians can perform multiple tasks, ranging from regular check-ups to medication management, and remotely monitor patient’s health status.
The ability to deliver such services remotely not only adds value to the patient’s care but also factors significantly into the billing for CCM.
It’s essential to classify the services correctly under telehealth while billing. This ensures proper compensation for services provided and helps avoid any compliance issues.
Coding for these services can differ based on the specific telehealth platform used, so investment in up-to-date coding education is key.
Monitoring telehealth usage is another important element in the billing process. Careful documentation of the telehealth services provided can help to maintain an accurate billing record and promote greater transparency during audits.
It’s pertinent to remember that only non-face-to-face telehealth services are eligible for CCM codes selection.
The transition to telehealth calls for an effective billing process, total compliance with Medicare regulations, and the provision of high-quality CCM.
Understanding these factors can significantly simplify your billing process, ensuring your practice reaps the full benefits of telehealth services.

What documentation is required for chronic care management billing?
The importance of accurate and detailed documentation in chronic care management billing cannot be overstated. Documents play an essential role in verifying the services that you provide to your patients and affirming their eligibility for these services.
Without proper paperwork, you may face difficulties in securing reimbursements, potentially impacting your practice’s revenue cycle.
Primarily, the patient’s medical records should include a comprehensive care plan. This plan should reflect the patient’s health problems, measurable treatment objectives, expected outcomes, and the medications and therapies involved. It should also demonstrate that the provider has engaged with the patient and, if applicable, any caregivers.
Besides, a formal agreement signed by the patient acknowledging and consenting to receive Chronic Care Management (CCM) services is requisite. Suppose the patient decides to revoke their agreement.
In that case, it should also be documented, including the date of revocation, as Medicare requires this documentation.
Moreover, documentation of the time spent providing CCM services is vital. All the non-face-to-face services provided during the calendar month should be logged in detail, with the total time accumulating to the minimum required, typically 20 minutes.
It’s significant to remember that your practice’s electronic health record (EHR) system may not automatically capture all these non-face-to-face services, thus manual documentation might be necessary.
Understanding Medicare’s chronic care management billing codes is also crucial. Each code corresponds to distinct services, and accurate documentation confirms the use of the correct billing code. This prevents potential overbilling or underbilling.
In conclusion, precise and comprehensive documentation is a crucial step in chronic care management billing. It ensures compliance, facilitates accurate billing, and fortifies the provider-patient relationship through transparent communication about the care provided.
How to ensure compliance in chronic care management billing?
Compliance is your key to the safe harbor in chronic care management billing. It demands a thorough understanding of regulatory guidelines and strict adherence to them.
But relax, you don’t have to navigate these choppy waters alone. Let’s break down some steps to help you ensure compliance.
Firstly, be familiar with the billing codes related to chronic care management (CCM). These codes – from 99490 to 99491 or 99487-99489 – can vary depending on the complexity and time spent on care. Misuse of these codes can result in denials or audits.
Therefore, it’s crucial to train your staff on accurate coding.
Next, keep the lines of communication open with your patients. Make sure your patients understand your CCM services and that they’re provided with a comprehensive care plan.
Remember the importance of obtaining a patient’s consent before initiating CCM services. This is not just good practice, but a mandatory requirement by Medicare.
Furthermore, document everything. From clinical summaries, patient-physician communication, to care management activities, each detail matters.
Every record should be not only meticulous but also easily retrievable. This invites transparency and maintains the integrity of your billing process, thus preventing potential compliance issues down the line.
Lastly, always stay updated with evolving CMS guidelines and policy changes. This could be changes in the reimbursement rates, modifications in the requirements for CCM, or an addition of a new billing code.
To sum up, compliance in chronic care management billing is a mix of diligent coding, clear communication with patients, meticulous documentation, and keeping a close eye on regulatory changes.
Done right, it’s your ticket to smooth sailing in the complex world of chronic care management billing.
Exploring the Opportunities in Chronic Care Management Revenue
Let’s dive deeper into the fascinating world of chronic care management revenue. Uncover the tremendous opportunities that lie beneath the surface, all designed to optimize your practice’s potential and boost your income.
Think about this. Incorporating Chronic Care Management (CCM) services into your healthcare practice could open up a whole new revenue stream.
Reimbursement for CCM services by Medicare can provide substantial additional revenue. This is particularly true if you have a significant portion of Medicare-eligible patients suffering from multiple chronic conditions.
In essence, you’re not adding more patients, but you’re providing more comprehensive care for your existing patients – and getting paid for it.
This approach not only enhances patient outcomes but also improves your bottom line.
Naturally, exploring such revenue options requires understanding the nuances of Medicare’s CCM billing and coding guidelines.
You’d need to put systems in place to document all the required service elements meticulously, whether provided in-office or via telehealth. Once you master these intricacies, however, the potential for revenue growth is genuinely enticing.
Another potentially lucrative aspect involves the use of technology. Innovative health technologies, especially care management software, can streamline billing processes, improve documentation, and ultimately increase revenue.
They reduce the time and resources spent on administrative tasks, allowing more focus on delivering quality patient care.
In a nutshell, venturing into chronic care management and making the most of the opportunities presented can significantly enhance your practice’s revenue.
All it takes is understanding the rules, leveraging the right technologies, and delivering the best possible patient care. It’s a win-win situation for both the healthcare provider and the patients they serve.
Approximately 117 million people in the U.S. have one or more chronic health conditions. Chronic diseases account for 75% of the nation’s healthcare spending.
Increasing Your Profitability with Chronic Care Management Services
Let’s face it, chronic care management (CCM) not only provides a vital service to patients but can also serve as a significant revenue generator for your practice.
To effectively increase your profitability with CCM services, you’ll need to follow a few key steps.
Firstly, you must optimize your operational efficiency. It’s crucial to minimize the administrative burdens of managing chronic diseases to keep your practice profitable. Structure your team so roles and responsibilities are clearly defined.
One approach may be to have your clinical staff focus on patient care, while your administrative staff manages the billing aspects of your CCM services.
Secondly, proactive patient identification is key. There’s a hidden goldmine of patients within your practice who could benefit from CCM services.
By identifying these patients and enrolling them in your CCM program, you’re not only improving their care, but also adding to your bottom line.
Thirdly, invest in technology that automates aspects of your process. An automated system can help keep patient records updated, track time spent on CCM services, and simplify billing.
This frees up your team’s time to focus on delivering high-quality patient care, while also ensuring every billable minute is accurately accounted for.
Last but certainly not least, continuously review and analyze your CCM program performance. Regular audits can help identify areas for improvement, allowing you to fine-tune your program and maximize profitability.
With careful planning and a strategic approach, implementing a successful and profitable CCM program is a realizable goal.
Remember, the better the care you provide for your chronically ill patients, the more you stand to benefit financially. That’s ultimately a win-win for both you and your patients.
For many healthcare providers, the reimbursement for CCM services lies in the range of $42 to $83 per patient per month.
However, the exact amount can fluctuate based on various key factors including the patient’s health conditions, the specific plans of the insurer, the intensity of care required, and the geographic location where the services are provided.
In essence, providers are reimbursed by Medicare using a CPT rate of about $42 for non-complex CCM that includes at least 20 minutes of clinical staff time.
Meanwhile, more complex care or higher time commitment could yank the reimbursement up to approximately $83.
These rates reflect the average payment for Medicare beneficiaries only, and the numbers may differ when billing other insurance providers.
It’s also important to remember that reimbursement rates are not set in stone. They are typically reviewed on a yearly basis and can change based on new policies, revised care guidelines, adjustments in healthcare costs, and other similar variables.
Therefore, it’s essential for healthcare practitioners to stay updated with the latest changes in billing codes and rates to ensure they are optimizing their reimbursement opportunities.
Lastly, using billing software can potentially enhance the efficiency of the billing process. These technologies can streamline data entry, manage insurance claims, and conduct billing audits, making the overall process quicker, easier, and more accurate.
Having such a system in place can help your practice ensure consistency in the billing process and reduce errors—ultimately leading to a more reliable reimbursement.
| Service | Monthly Fee per Patient | Annual Revenue (For 100 Patients) |
|---|---|---|
| Chronic Care Management (CCM) | $42 | $50,400 |
| Complex Chronic Care Management | $83 | $99,600 |
| General Behavioral Health Integration | $48 | $57,600 |
| Pyschiatric Collaborative Care Model | $141 | $169,200 |
Outsourcing Chronic Care Management Billing: Pros
Are you finding it difficult to navigate the complex landscape of chronic care management (CCM) billing? If so, then outsourcing might just be the solution you’re looking for.
By delegating the intricacies of CCM billing to a third-party expert, you can experience a range of benefits.
First, financial efficiency is a significant advantage of outsourcing. Engaging a specialized billing service can lead to cleaner claims, faster payments, and fewer unpaid services, which boost your bottom line over time.
With the knowledge and resources to keep up with legislative changes and insurers’ policies, high-quality billing service providers can help you avoid costly denials or underpayments.
Second, outsourcing CCM billing lets you focus on patient care. When you’re not tangled up in administrative tasks, you’re free to devote more time and energy to what truly matters: your patients.
Good companies provide comprehensive services that leave you free to concentrate on practice.
Third, you can significantly reduce errors that might lead to unnecessary financial losses or regulatory penalties. Experienced billing professionals are proficient in coding and following up on claims, adept at identifying areas of potential concern, and equipped to take immediate corrective action.
Finally, technology adoption is another compelling reason. Billing companies generally use advanced software to assure that billing is accurate, swift, and compliant with regulations. Besides, they usually keep themselves updated with the latest billing technology trends.
Outsourcing billing for CCM services can help reduce your administrative cost by 40% to 50%.
In essence, outsourcing CCM billing can be a strategic decision to improve your cash flow, enhance patient care, minimize billing errors, and take advantage of modern technology. But, as with any decision, it’s important to weigh the pros and cons according to your individual practice’s needs.
So to wrap up we have discussed:
Chronic Care Management (CCM) services are billable under Medicare Part B.
Now lets talk about what are the common mistakes in chronic care management billing and how to avoid them?
Chronic care management billing is an intricate process that should be navigated with precision. One common mistake in this process is under-coding – which is understating the complexity or extent of care provided. This mistake can inadvertently lead to reduced reimbursement.
To circumvent this, double-check your documentation for all care activities and ensure you are accurately coding for everything that was provided.
Another frequent slip-up is not tracking the time allocated to care management adequately. Remember, time is a critical component in chronic care management billing as most codes are time-based.
Use time tracking tools or electronic health record (EHR) features to accurately document the time spent on healthcare services.
Additionally, you should ensure that the documentation of non-face-to-face services is adequate and the time spent on such services is being accounted for and billed correctly.
Overlooking patient consent is another major mistake that could bring unwelcome legal troubles. Under both Medicare and private payer guidelines, patients must give their consent before you can bill for chronic care management services.
Consent can be oral or written, but it’s always safest to get a written agreement. This not only provides legal protection but also helps educate the patient about their care and the associated costs.
Lastly, keep an eye out for any changes in billing codes or insurance policies. Keeping up-to-date with the latest guidelines and changes can prevent financial loss and ensure smooth operation for both patients and your practice.
Neglecting new CPT (Current Procedural Terminology) updates, for instance, could mean overlooking opportunities for increased revenue.
Therefore, maintaining communication with the rest of your healthcare team and constant monitoring of updates is critical in this aspect.
Managing chronic care billing can indeed be quite challenging, but by staying vigilant for these common mistakes and implementing these corrective strategies, you can steer clear of potential pitfalls and ensure a smooth, compliant billing process.
How does chronic care management billing vary with different insurance providers?
When it comes to chronic care management billing, the approach can vary significantly across different insurance providers.
This range in practices often stems from differences in policy guidelines, rate structures, and coding preferences.
Let’s delve into these nuances to give you a better understanding.
The primary factor contributing to the disparity is each provider’s unique policy guidelines. Some insist on detailed documentation, while others may be more lenient in accepting general information.
For example, certain insurance companies need substantial proof of the chronic conditions being managed, requiring diagnostic tests and comprehensive patient records.
Others might just require a straightforward doctor’s report briefly stating the condition and treatment plan.
Payment rates is another area where differences emerge. Contrary to popular belief, not all insurance companies pay the same rate for the same service.
It’s critical that you thoroughly understand the rate structure of the individual insurance providers you’re working with, as this can drastically impact your returns.
Finally, billing codes can also deviate across insurers. Different insurance providers may use slightly varying codes for chronic care management services, meaning that incorrect coding can lead to delayed or denied claims.
This coding standard can be especially tricky when dealing with Medicare and Medicaid services, which have their own set of unique codes.
To sum up, understanding the varying insurance provider practices in chronic care management billing is crucial for accurate processing and maximizing revenue.
Invest time to familiarize yourself with different policy norms, rate structures, and coding preferences, and you’ll soon find this process becomes simpler.
If you have any question reach us at rxcredentialin.com or you can also call during business hour on 716-919-3969.
Thank you.