DME Supplier Credentialing Service
We help DME suppliers get properly enrolled, credentialed, and contracted so you can bill confidently, reduce compliance risk, and accelerate reimbursements — without portal headaches or missing paperwork.
- ✓ Medicare supplier enrollment support
- ✓ Commercial payer contracting guidance
- ✓ Credential packet + document organization
- ✓ Proactive follow-ups to prevent delays
- ✓ EFT/ERA setup assistance (as needed)
- ✓ Ongoing updates & revalidation tracking

Fast submissions • Dedicated follow-ups
What Sets Us Apart
DME supplier credentialing has higher scrutiny than standard provider enrollment — from supplier standards and documentation to payer-specific requirements. Our team keeps your submissions clean, complete, and compliance-ready, and we proactively follow up so you don’t lose revenue from avoidable delays. For Medicare-aligned requirements, we follow guidance tied to the CMS provider enrollment framework, and we align credential files to payer expectations and credentialing best practices.
DME-Specific Documentation Readiness
We organize and validate the core supplier documents payers typically request so your application is complete the first time.
Cleaner Submissions, Fewer Holds
We reduce common credentialing “stall points” by tightening ownership details, identifiers, supporting files, and required attestations.
Proactive Follow-Ups Until Final Outcome
We track the application status, respond to payer requests quickly, and keep the process moving until you receive final confirmation.
Credentialing + Revenue Support Options
Need help beyond enrollment? We also support revenue-side services like AR recovery and denial management.
How It Works
We run a structured credentialing workflow designed for DME suppliers: collect and verify supplier details, prepare a payer-ready credential file, submit applications, and follow up until you’re approved and ready to bill. Where applicable, we use Medicare-aligned enrollment concepts and documentation references from the NPPES (NPI Registry) to ensure identifiers and business details are consistent across systems.
Step 1: Supplier Profile & Document Intake
We gather your business details, ownership information, identifiers, and core compliance documents needed for payer enrollment.
Step 2: Credential File Review
We QA everything for accuracy (names, addresses, tax IDs, NPIs, supporting files) to reduce requests for corrections.
Step 3: Payer Submissions
We submit payer applications based on your target networks and service footprint, following each payer’s submission rules.
Step 4: Follow-Ups & Final Confirmation
We handle payer communications, provide any additional documentation requested, and confirm approval and effective dates.
Benefits of Outsourcing
DME Supplier Credentialing
Faster Medicare Enrollment
Cut CMS-855S processing time from 6 months to 30-60 days with our error-free submissions.
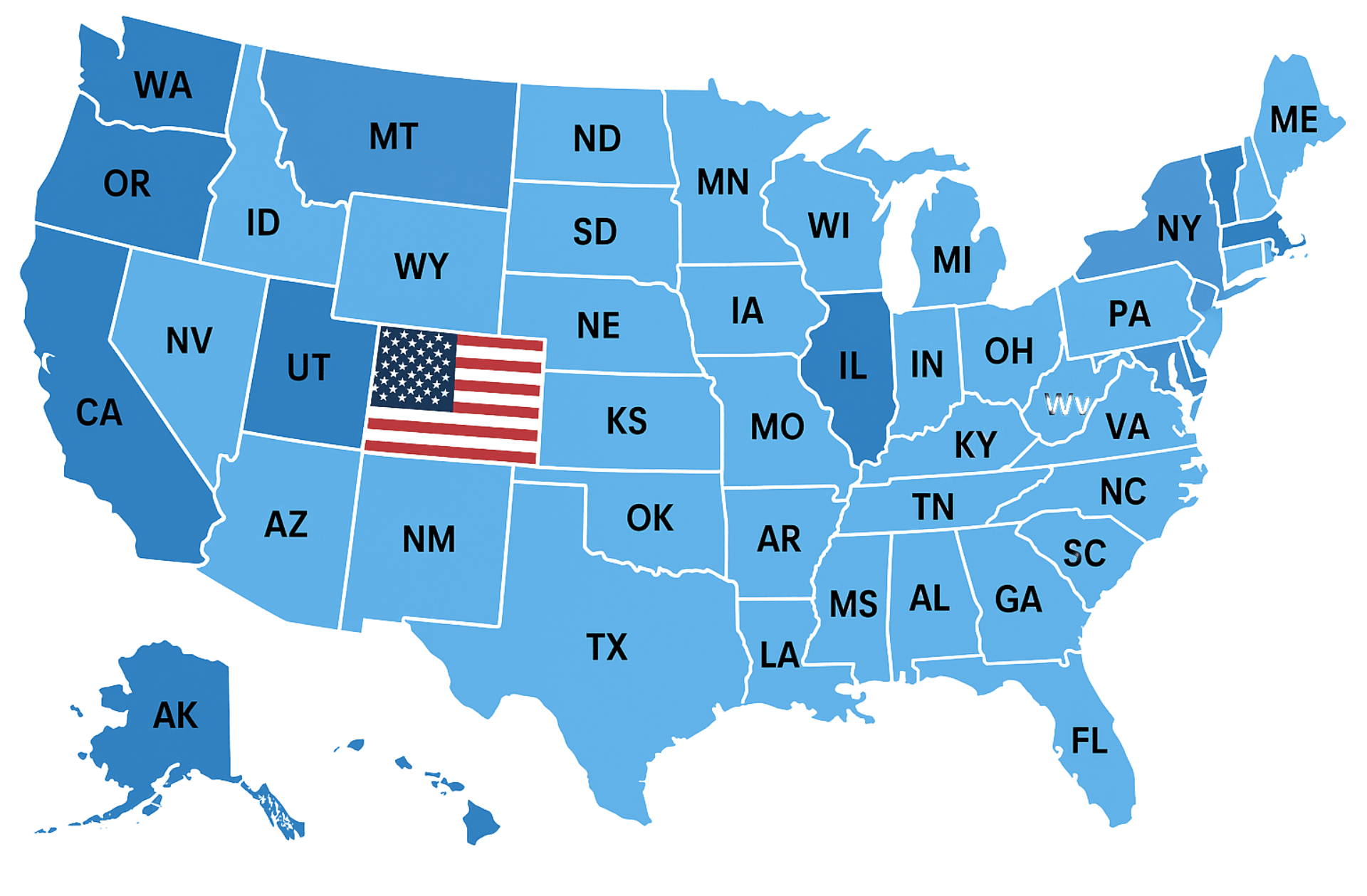
Multi-State Licensing
Navigate varying state DME requirements and facility inspections across all 50 states.
Product-Specific Credentialing
Proper HCPCS mapping for orthotics, respiratory, wound care, and other DME categories.
Payer Contract Negotiation
Secure optimal reimbursement rates with private insurers and Medicare Advantage plans.
Accreditation Compliance
Ensure ACHC, Joint Commission or CMS accreditation requirements are met.
Continuous Revalidation
Automatic tracking of Medicare revalidation deadlines and license renewals.
Audit Documentation
Maintain CMS-compliant proof of delivery systems and supplier standards.
Revenue Acceleration
Begin billing 3-5 months sooner compared to in-house credentialing.
Staff Efficiency
Free up your team to focus on patient care rather than paperwork.
Have Other Questions? Get in Touch!
Our team is ready to guide you through every step of credentialing, contracting, and payer enrollment, making the process fast, simple, and stress-free.
The industry-standard timeline is 60 to 90 business days in most cases.
You get a dedicated credentialing manager who guides you and keeps you updated at every step.
No. You should wait for contract approvals before seeing patients.
We will need your state license, DEA, board certification, malpractice insurance, EIN Letter and a voided check to begin with the process.
We charge $140 per commercial application and $199 per government payer application. We do not charge any fee for closed panels.
Insurance Companies We Work With
We work with every health plan in the United States, including Medicare, Medicaid, major commercial carriers like Aetna, Cigna, Humana, Blue Cross Blue Shield, UnitedHealthcare, as well as HMO, PPO, POS, state, and regional plans. Our team ensures seamless credentialing and contracting across all payers.
Trusted by Healthcare Providers Nationwide












Very attentive and efficient
Always available to explain things or answer questions or concerns












We would love to hear from you.
Contact Us
Have a question or want to learn more about our services? Fill out the form below and our team will get back to you within 24 hours.
We serve all 50 states.