Behavioral Health Billing Services Built for Therapy & Psychiatry
We manage end-to-end billing for outpatient behavioral health practices — eligibility checks, clean claim submission, denial management, and AR follow-ups — so you can focus on clients, not collections.
Verify benefits before the visit
Reduce surprises, improve collections, prevent avoidable denials.Fix, appeal, and resolve rejections
We track payer rules, resubmit quickly, and prevent repeat issues.Chase aged claims the right way
Consistent follow-ups so older balances don’t become write-offs.Expand payer networks faster
Enroll providers correctly to start billing in-network sooner.Every Step of Your Billing Process Managed for You
Our team manages the entire billing process for you, including claim preparation, scrubbing submission, tracking, and denial resolution. With proven workflows built for small practices, we help you improve cash flow, reduce errors, and maintain complete visibility into your revenue at every step.
- Encounters Review
- Claim Preparation
- Coding Accuracy Review
- Batch Claim Submission
- Real Time Status Tracking
- Weekly Follow Ups
- Denial Resolution
- Accounts Receivable Management
- EDI, ERA and EFT Setup
- Support for All EHR Systems
What Sets Us Apart
Behavioral health billing has unique denial triggers — eligibility mismatches, authorization gaps, telehealth rules, POS modifiers, and documentation requirements. We work directly inside your existing EHR/billing workflow (no forced software changes) and track every claim from submission to payment. You get clear visibility into pending claims, payments, allowed amounts, and denials — plus specific guidance to prevent repeat issues. Need credentialing support for new therapists or prescribers? Explore our insurance credentialing services.
Behavioral Health Coding Accuracy
We scrub claims for common BH risk points (telehealth POS/modifiers, rendering/billing NPI setup, and payer-specific rules) to reduce preventable denials.
Authorization & Eligibility Support
We help your front desk verify benefits and auth requirements so visits are billed correctly and patient responsibility is clearer.
Denial Management That Prevents Repeat Issues
Denied claims are corrected and appealed quickly, with root-cause tracking to stop the same denial patterns from happening again.
AR Follow-Up & Recovery
Aged claims are worked consistently with payer follow-ups so clean revenue doesn’t become write-offs. See our AR recovery services.
Full Team Coverage (Not One Biller)
You get a structured team approach with documented workflows — so billing doesn’t stall if one person is out.
Fast, Reliable Communication
Questions and updates are handled quickly with simple reporting that shows what was submitted, paid, denied, and pending.
Payer Rule Guidance for BH & Telehealth
We keep you aligned with payer policies for behavioral health, including telehealth billing nuances and documentation expectations.
Integrated Credentialing + Billing Support
If you’re adding providers or expanding payers, we align billing setup with enrollment status so you don’t bill under the wrong contracts.
How It Works
Our onboarding is designed to be fast and low-friction — typically completed in three to five business days — so your practice keeps running without downtime. We configure billing settings, confirm payer connectivity, and start submitting clean claims immediately.
Practice Intake & Workflow Mapping
We gather core details (providers, locations, payer mix, telehealth vs in-person) and map your current intake-to-claim workflow.
Credentialing & Payer Participation Check
We verify each clinician’s payer participation to prevent out-of-network billing mistakes. If needed, we coordinate with credentialing services.
EHR + Billing Setup
We configure billing/rendering providers, payers, and claim settings inside your system to ensure claims generate correctly.
EDI/ERA & Payment Posting Readiness
We confirm EDI claim routes and ERA posting workflows so payments and EOBs reconcile quickly and cleanly.
Charge Setup & Behavioral Health Rules
We validate your charge setup and billing rules so claims match payer requirements (including telehealth configurations where applicable).
Daily Billing Operations Begin
We submit claims, track responses, work denials, and follow AR — with consistent updates so you always know what’s happening.
Have Other Questions? Get in Touch
Our team is here to help you understand every part of the billing process, from claim submission to reimbursement. Whether you need clarity on workflows, payer rules, or how our services fit your practice, we make the entire experience simple, transparent, and stress-free.
Our onboarding process is completed within 3–5 business days, provided all required information is supplied.
Yes — we work with nearly all popular platforms such as Tebra, OfficeAlly, eCW, Athena, DrChrono, AdvancedMD, SimplePractice, ICANotes, Optimantra, and more.
Our base plan starts at $499/month and includes free credentialing for solo practitioners. Standard billing plans are 3–5% of insurance collections.
Yes — we offer free credentialing, CAQH maintenance, and revalidation support for billing clients.
All PHI is handled in accordance with HIPAA requirements. Our team uses secure, encrypted systems for file storage, communication, and data access. Access to PHI is limited to authorized staff only, based on job responsibilities, and all activity is monitored.
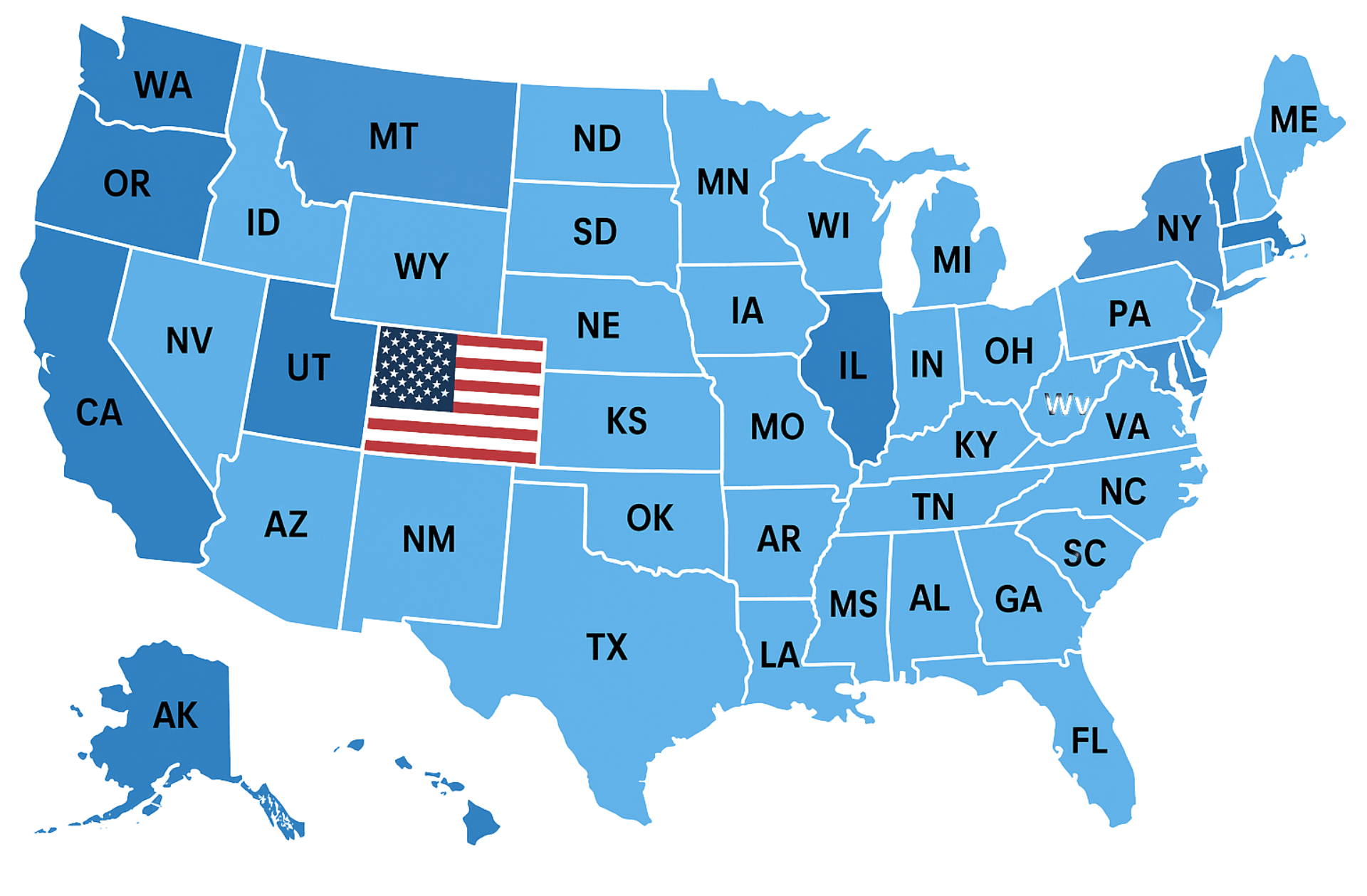
Insurance Companies We Work With
We work with every health plan in the United States, including Medicare, Medicaid, major commercial carriers like Aetna, Cigna, Humana, Blue Cross Blue Shield, UnitedHealthcare, as well as HMO, PPO, POS, state, and regional plans. Our team ensures seamless credentialing and contracting across all payers.
Trusted by Healthcare Providers Nationwide












Very attentive and efficient
Always available to explain things or answer questions or concerns












We would love to hear from you.
Contact Us
Have a question or want to learn more about our services? Fill out the form below and our team will get back to you within 24 hours.
We serve all 50 states.