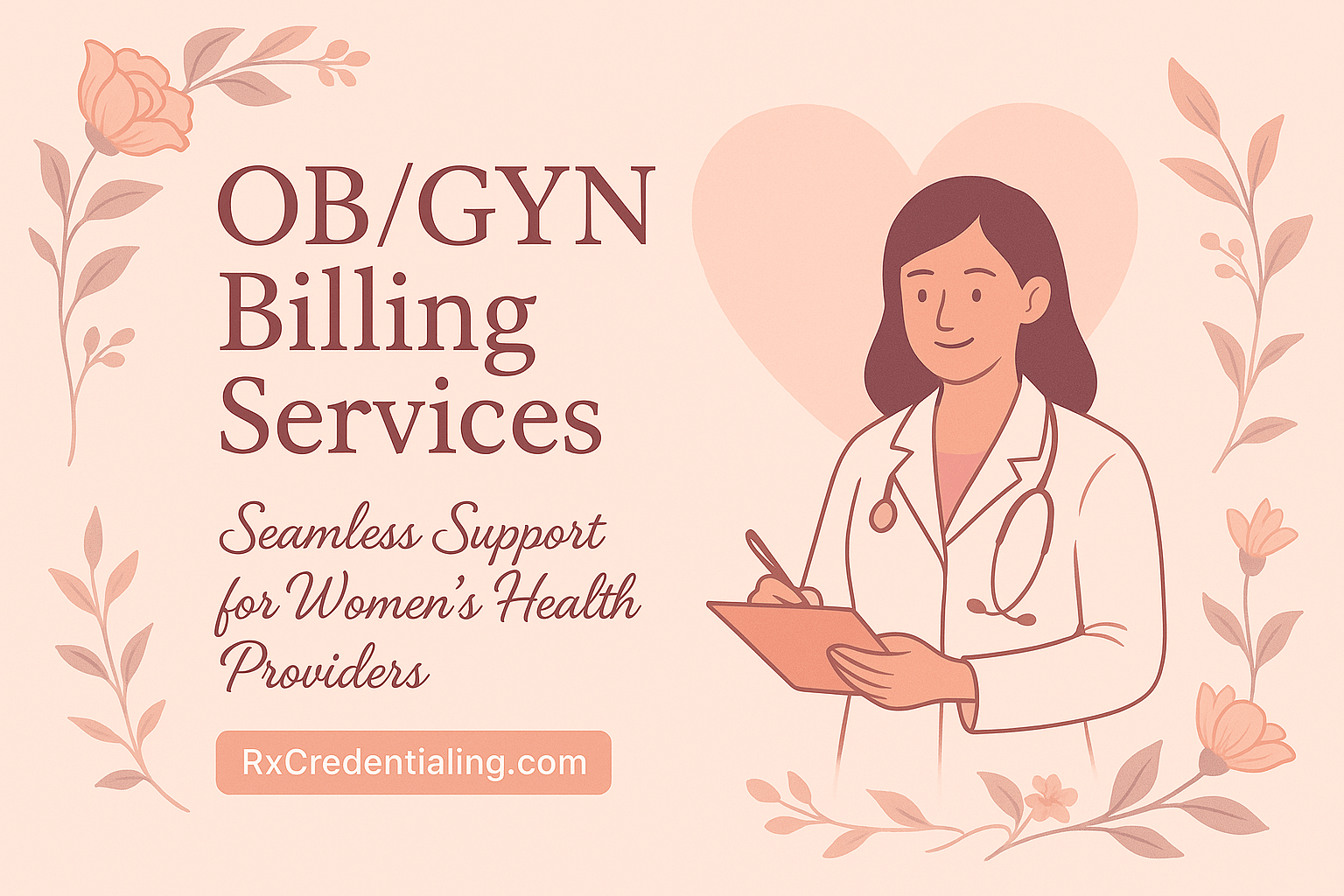
OB/GYN Billing Services
OB/GYN billing involves global maternity packages, prenatal/postpartum visit rules, ultrasound coding, contraception, and payer-specific authorization requirements. We manage the full revenue cycle so you reduce denials, protect reimbursements, and get paid on time.
- ✓ Global OB Package Billing
- ✓ Ultrasound & Procedure Coding
- ✓ Prior Auth & Referrals Support
- ✓ Denial Appeals & Reprocessing
- ✓ AR Follow-Up & Recovery
- ✓ Real-Time Reporting
Free Credentialing with Medical Billing
$499 / Month
Call / WhatsApp:
(716) 919-3969
Email:
support@rxcredentialing.com
www.rxcredentialing.com
Ob/gyn
Medical Billing Services
- ✅ Smooth transition between EHR/EMR systems.
- ✅ Efficient Electronic Funds Transfer (EFT), EDI, and ERA setups.
- ✅ Claims submission within 24 hours.
- ✅ Prompt follow-up with payers for faster reimbursements.
- ✅ Free CAQH maintenance and provider revalidation.
- ✅ Comprehensive Revenue Cycle Management (RCM) services.
- ✅ Appeals, adjustments, and coding review included.
- ✅ Referral coordination with other practices and specialists.
- ✅ Reimbursement strategies for optimized billing.
What Sets Us Apart
OB/GYN revenue is often impacted by global maternity billing timing, incomplete documentation for prenatal/postpartum services, authorization gaps, and payer rules around ultrasounds and procedures. We tighten workflows, scrub claims for OB/GYN-specific rules, and manage denials until resolution. For payer documentation and “who should pay” issues, we can also support eligibility verification. For general guidance on preventive service coverage rules, we reference Women’s preventive services coverage.
Global OB Package Expertise
We manage global maternity billing timelines and visit capture so you’re reimbursed correctly across the full episode of care.
Procedure + Ultrasound Coding Accuracy
We scrub claims to reduce rejections tied to coding, modifiers, place of service, and payer-specific edits.
Authorization & Referral Support
We track auth requirements for imaging and procedures and help prevent denials caused by missing approvals.
Denials + AR Worked Consistently
We resolve denials, appeal when needed, and work aged claims so payable revenue doesn’t sit in AR.
How It Works
We follow a structured OB/GYN billing workflow: learn your services and payer mix, confirm EHR and clearinghouse configuration, standardize eligibility and auth checks, then run daily billing with tracking and reporting. If you need additional help after posting, we can pair billing with AR recovery services to clean up aging balances.
Step 1: Intake & OB/GYN Workflow Review
We review your visit types, maternity workflow, imaging/procedure volume, payer mix, and common denial patterns.
Step 2: EHR / Clearinghouse Setup
We confirm provider profiles, NPIs, taxonomy, payer IDs, EDI/ERA, and claim rules so submissions are clean.
Step 3: Daily Claim Operations
Charge entry, claim scrubbing, submissions, rejection handling, payment posting, and patient balance workflows.
Step 4: Denials, Appeals, Reporting
We work denials and AR, identify root causes, and apply prevention steps with clear reporting you can review anytime.
Have Other Questions? Get in Touch
Our team is here to help you understand every part of the billing process, from claim submission to reimbursement. Whether you need clarity on workflows, payer rules, or how our services fit your practice, we make the entire experience simple, transparent, and stress-free.
Our onboarding process is completed within 3–5 business days, provided all required information is supplied.
Yes — we work with nearly all popular platforms such as Tebra, OfficeAlly, eCW, Athena, DrChrono, AdvancedMD, SimplePractice, ICANotes, Optimantra, and more.
Our base plan starts at $499/month and includes free credentialing for solo practitioners. Standard billing plans are 3–5% of insurance collections.
Yes — we offer free credentialing, CAQH maintenance, and revalidation support for billing clients.
All PHI is handled in accordance with HIPAA requirements. Our team uses secure, encrypted systems for file storage, communication, and data access. Access to PHI is limited to authorized staff only, based on job responsibilities, and all activity is monitored.
Insurance Companies We Work With
We work with every health plan in the United States, including Medicare, Medicaid, major commercial carriers like Aetna, Cigna, Humana, Blue Cross Blue Shield, UnitedHealthcare, as well as HMO, PPO, POS, state, and regional plans. Our team ensures seamless credentialing and contracting across all payers.
Trusted by Healthcare Providers Nationwide












Very attentive and efficient
Always available to explain things or answer questions or concerns












We would love to hear from you.
Contact Us
Have a question or want to learn more about our services? Fill out the form below and our team will get back to you within 24 hours.
We serve all 50 states.