Physical Therapy Credentialing Services
We help PT clinics and rehab providers enroll with Medicare, Medicaid, and commercial insurance plans—so you can expand in-network access, reduce out-of-network friction, and start billing with confidence.
- ✓ CAQH setup & maintenance
- ✓ Medicare & Medicaid enrollment
- ✓ Commercial payer contracting
- ✓ Ownership & location updates
- ✓ Fast follow-ups + status tracking
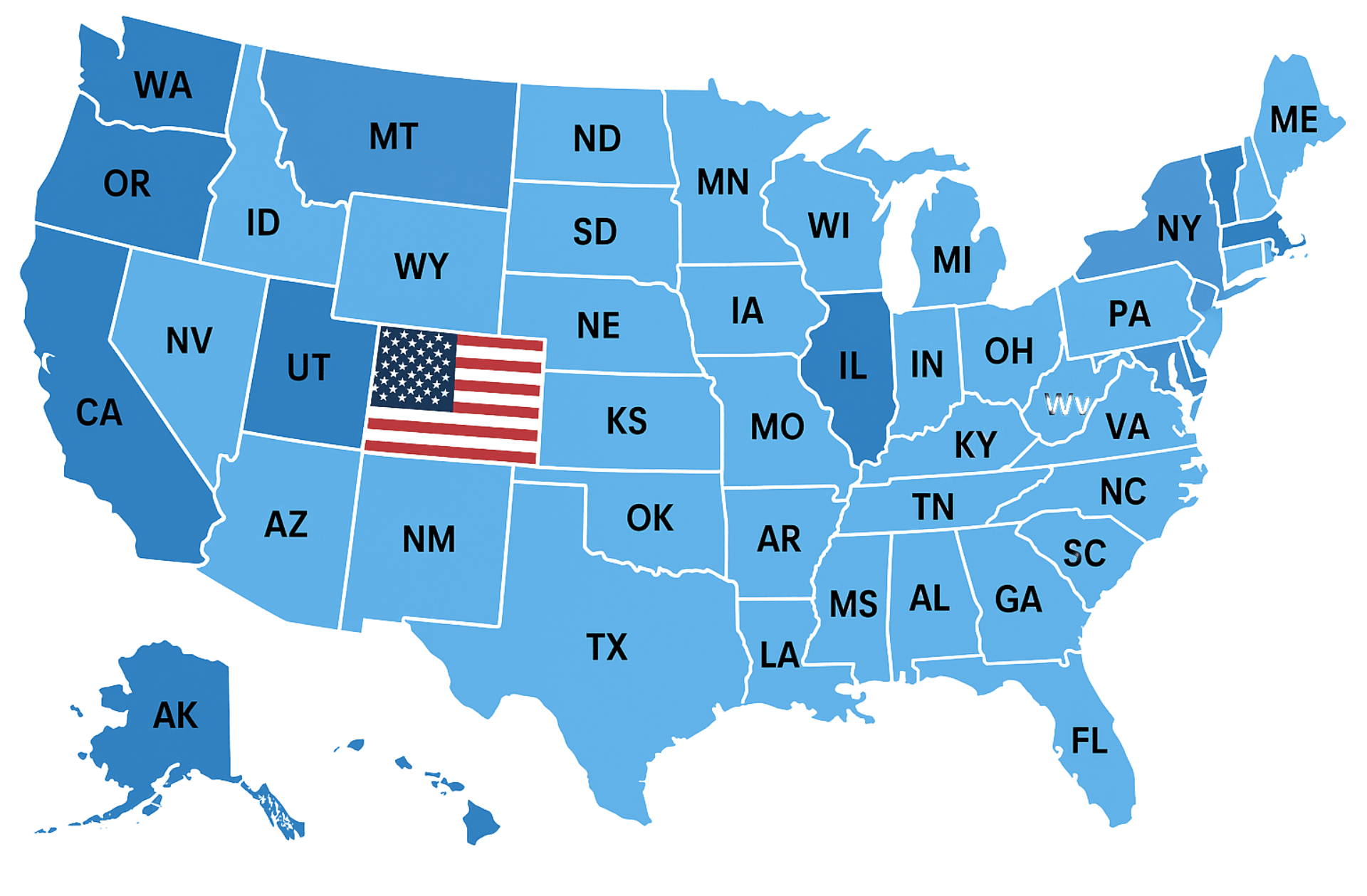
- ✓ Nationwide credentialing support
What Sets Us Apart
Physical therapy credentialing can stall due to small mismatches (practice NPI vs. rendering NPI, taxonomy, service locations, CAQH documents, and ownership details). We keep your PT credentialing file clean, consistent, and payer-ready—then follow up until you receive final confirmation and effective dates. To keep identifiers aligned across systems, we validate details using the NPPES (NPI Registry) and apply credentialing best-practice workflows used by major payers.
PT-Focused Payer Strategy
We help you choose the right payer mix for your PT clinic—based on location, services, and patient demand—so you credential with plans that drive volume.
CAQH Accuracy + Consistency Checks
We ensure your CAQH profile matches payer applications (addresses, taxonomy, licenses, malpractice, W-9) to prevent avoidable holds.
Proactive Follow-Ups Until Final Outcome
We track your application status, respond to payer requests quickly, and keep your file moving until approval confirmation is received.
Support Beyond Credentialing
After you’re in-network, we can support the revenue side with eligibility verification and AR recovery to protect cash flow and reduce preventable denials.
How It Works
We run a structured credentialing workflow designed for PT practices: collect and verify clinic/provider details, build a payer-ready credential file, submit applications, and follow up until you are approved and ready to bill. Where payer rules reference Medicare-style enrollment concepts, we align documentation to the CMS provider enrollment framework to keep your practice information consistent across systems.
Step 1: Intake & Clinic Setup
We collect your PT clinic details, service locations, NPIs, taxonomy, licenses, malpractice, W-9, and EIN/voided check (if applicable) plus payer targets.
Step 2: CAQH + Application QA
We update/confirm CAQH, validate details across every form, and fix common mismatch issues before submission to reduce delays.
Step 3: Payer Submissions
We submit your PT credentialing applications through payer portals or paper workflows and document submission proof for tracking.
Step 4: Follow-Ups, Contracting, Effective Dates
We handle payer communications, provide additional documentation when requested, and confirm approvals, effective dates, and next steps for billing readiness.
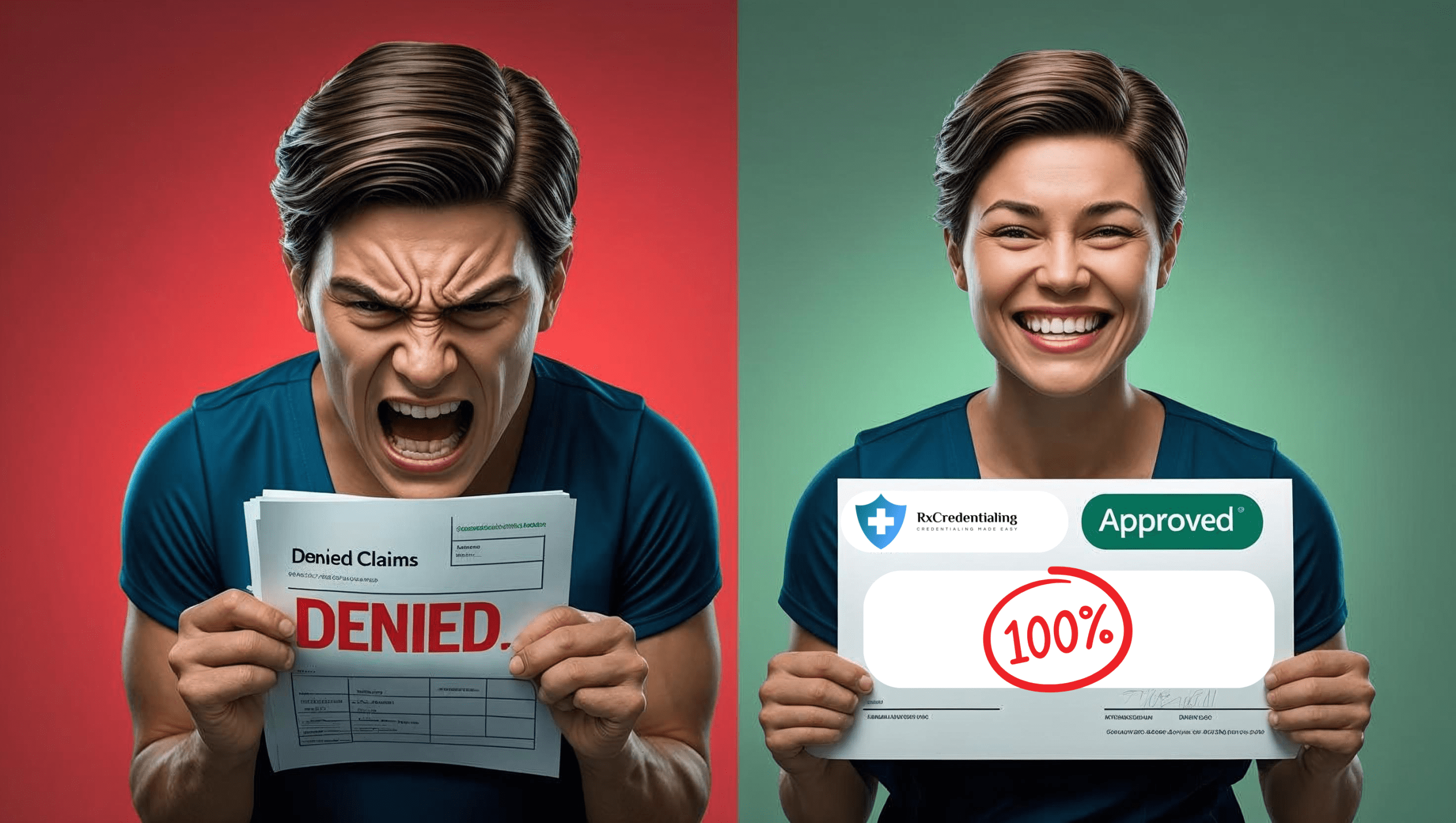
Benefits of Outsourcing
Physical Therapy Credentialing
Faster PTAN Approval
Get credentialed with Medicare in 30 days (vs. 60-90 day average) to start billing sooner
Dry Needling Coverage
Proper enrollment for 20560/20561 codes with correct modifiers to prevent denials
Multi-Location Credentialing
Structure PTANs correctly across clinics to avoid CMS reassignment penalties
Specialty Program Enrollment
Expedited credentialing for LSVT BIG, vestibular rehab, and pelvic health programs
Higher Reimbursement Rates
Identify and enroll with highest-paying PT insurance plans in your area
Workers' Comp Optimization
State-specific credentialing for industrial rehab cases with pre-negotiated visit limits
Telehealth Credentialing
Proper enrollment for virtual PT services with location-02 requirements
Audit Protection
CMS-compliant documentation for functional limitation reporting (G-codes)
8-Minute Rule Compliance
Proper credentialing for timed codes with built-in billing calculations
Have Other Questions? Get in Touch!
Our team is ready to guide you through every step of credentialing, contracting, and payer enrollment, making the process fast, simple, and stress-free.
The industry-standard timeline is 60 to 90 business days in most cases.
You get a dedicated credentialing manager who guides you and keeps you updated at every step.
No. You should wait for contract approvals before seeing patients.
We will need your state license, DEA, board certification, malpractice insurance, EIN Letter and a voided check to begin with the process.
We charge $140 per commercial application and $199 per government payer application. We do not charge any fee for closed panels.
Insurance Companies We Work With
We work with every health plan in the United States, including Medicare, Medicaid, major commercial carriers like Aetna, Cigna, Humana, Blue Cross Blue Shield, UnitedHealthcare, as well as HMO, PPO, POS, state, and regional plans. Our team ensures seamless credentialing and contracting across all payers.
Trusted by Healthcare Providers Nationwide












Very attentive and efficient
Always available to explain things or answer questions or concerns












We would love to hear from you.
Contact Us
Have a question or want to learn more about our services? Fill out the form below and our team will get back to you within 24 hours.
We serve all 50 states.