Understanding the financial and operational investment required for medical credentialing is vital for the long-term success of your practice. This guide provides a detailed breakdown of all the factors that contribute to the total cost, helping you make a strategic decision for your business.
Unpacking the Costs: Why Credentialing is More Than a Single Fee
When you ask, "How much does medical credentialing cost?", the answer is rarely a simple number. The true cost is a multifaceted equation that includes not just a direct fee, but also time, expertise, and the potential for costly errors. Whether you are a solo practitioner, a multi-physician group, or a specialized practice like telehealth for counselors, understanding these factors is the key to a healthy financial outlook.
The process of medical credentialing is a complex and time-consuming administrative task that is non-negotiable for any practice wishing to bill insurance companies. It involves a series of steps to verify a healthcare provider's qualifications, including their education, training, licensure, and professional history.
Failing to complete this process correctly and efficiently can lead to significant delays in payment, claim denials, and a substantial loss of revenue. This article will dissect the various components of credentialing costs, compare in-house versus outsourced solutions, and provide a clear roadmap for success.
The Main Activities That Determine the Cost
The cost of medical credentialing is directly tied to the complexity and number of tasks that must be performed. These activities require specialized knowledge and meticulous attention to detail to ensure accuracy and compliance. Here is a breakdown of the core functions that a credentialing specialist handles, each contributing to the overall cost.
Initial CAQH Profile Setup & Maintenance
This involves the initial setup, completion, and ongoing maintenance of a provider's CAQH ProView profile. This is the central repository for all provider data and is a critical first step for most payers. Keeping it current is essential to prevent application delays and denials. For more on this, see our guide on mastering CAQH credentialing.
Payer Credentialing & Contracting
Credentialing for new payers is a key activity, especially for a new physician joining a medical practice. It involves submitting an application, following up with the payer, and securing an in-network contract. This also includes negotiating with insurance companies to get favorable rates for your practice. Find out more about healthcare payer contract negotiations.
Re-credentialing & Re-validations
Payer re-validations and re-credentialing, including for major government payers like Medicare and Medicaid, are required periodically. This process ensures a provider remains in good standing and continues to receive reimbursements. For more details, read our article on what is medical re-credentialing.
Document Expiration Tracking
This involves tracking the expiration dates for a physician's crucial documents, such as their medical license, malpractice insurance, and DEA registration. A missed renewal can lead to an interruption in billing. For example, a single provider's NPI registration requires attention to detail to ensure it's up to date.
Practice & Payer Roster Maintenance
Adding and deleting physicians to and from a medical practice is a frequent task that requires updating payer rosters. This ensures that new providers can bill immediately and that leaving providers are removed to prevent fraudulent claims. For a detailed guide on this, check out our article on how to complete the CMS-588 form.
NPI & Direct Deposit Setups
This includes tasks like NPI registration, direct deposit setups, and EIN confirmation, all of which are critical for receiving payments promptly. Correctly managing these ensures smooth revenue cycle management.
In-House vs. Outsourced: A Cost-Benefit Analysis
The most significant decision a practice faces is whether to handle these tasks in-house or to outsource them to a specialized service. While both options have their pros and cons, a clear understanding of the costs associated with each is the first step toward making a strategic choice.
In-House Credentialing Costs
For a practice with 10 physicians, hiring a full-time, experienced credentialing specialist seems like a straightforward solution. However, the costs extend far beyond a monthly salary.
The average salary for a credentialing specialist with at least 5 years of experience can easily be **USD 4,000 per month**. But this is just the beginning. According to the Bureau of Labor Statistics, employer costs for employee compensation can add an additional 30% to the base salary. In states like California or New York, where healthcare salaries and costs of living are higher, this number can be even greater.
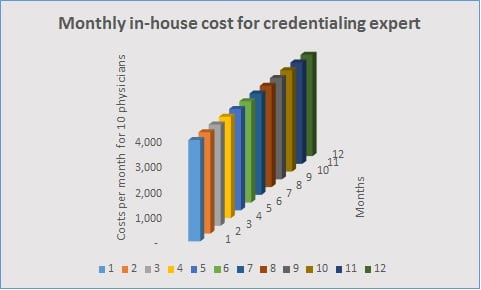
Here's a breakdown of the hidden costs:
- Salary & Benefits: Minimum USD 4,000/month, plus payroll taxes, health insurance, and retirement contributions.
- Training & Management: Time and resources spent on training, professional development, and managing the employee.
- Infrastructure: Costs for a workstation, software licenses, IT support, and other office overhead.
- The Cost of Errors: A single mistake can lead to months of payment delays, a huge hit to your revenue cycle management, and a significant loss of income for the practice.
Total estimated monthly cost: Over USD 5,200.
Outsourced Credentialing Costs
Outsourcing is a trending option for practices seeking to minimize costs and maximize efficiency. It provides access to a team of experts without the burden of a full-time employee, benefits, and infrastructure costs. With a service like Rxcredentialing, you can get providers credentialed with as many payers as you need.
The cost structure is simple and transparent. Our service is designed to get your providers credentialed with all major payers in your area within a typical six-month timeframe.
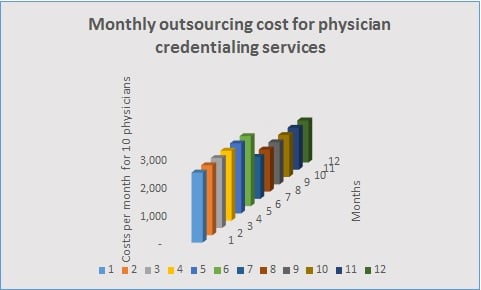
For an initial credentialing period, you might pay **USD 250 per month per provider.** For a practice with 10 physicians, that’s USD 2,500 per month. After all practitioners are credentialed, the cost can drop to a lower maintenance fee, for example, **USD 150 per month per provider.**
Let's calculate the total cost for the first year with 10 physicians:
- Initial Credentialing (6 months): $250/provider/month × 10 providers × 6 months = $15,000
- Ongoing Maintenance (6 months): $150/provider/month × 10 providers × 6 months = $9,000
Total estimated first-year cost: USD 24,000.
This brings your total first-year cost to **$24,000**, which is significantly less than the in-house option, which could easily exceed $60,000 in a year. Subsequent years would be even cheaper, with costs dependent on the number of new providers joining your practice.
The Cost of Getting It Wrong: Hidden Financial Risks
The biggest risk in a DIY or in-house approach is the potential for errors. A single mistake in a CAQH profile, a missed re-credentialing deadline, or a delayed application can trigger a domino effect of negative consequences, all of which come with a steep price tag.
According to a study by HFMA, administrative complexities and errors can cost the U.S. healthcare system billions of dollars annually. For an individual practice, these errors can be devastating.
The Ripple Effect of Credentialing Errors
- Delayed Revenue: A common credentialing error can delay a provider's ability to bill an insurance company for months, creating a significant gap in your practice's cash flow.
- Claim Denials: Incomplete or inaccurate credentialing information is a leading cause of claim denials. Each denied claim requires additional staff time to research, correct, and resubmit, leading to a cycle of rework. This is a key reason why practices turn to our healthcare denial management services.
- Administrative Overload: When credentialing is not handled properly, your administrative staff becomes overwhelmed with follow-up calls, paperwork, and payer communication, diverting their attention from other critical tasks. This is where virtual medical assistant services can also play a crucial role.
- Loss of Patients: If a provider is not properly credentialed, a patient with a specific insurance plan, such as those with HMO or PPO plans, may be unable to see them, forcing them to find another practice.
The cost of doing it wrong is not just the lost revenue but also the lost opportunity and the damage to your practice's reputation. Choosing the right partner means you get it right the first time, protecting your revenue and your peace of mind.
How to Minimize Costs by Choosing the Right Credentialing Company
You can only minimize these costs by choosing the right provider credentialing company. The best partner for your practice will not only handle the paperwork but will also act as a strategic advisor. When evaluating a potential partner, look for the following qualities.
A Checklist for Vetting a Credentialing Service
- Timely Follow-ups: The credentialing process is a waiting game, and a good service will have a system for consistent, timely follow-ups with payers to keep the process moving.
- Payer Expertise: They should be capable of advising you on the best payers in your location, helping you prioritize applications to maximize your patient base and revenue. This is a core part of what we offer for our chiropractic practices and nurse practitioners.
- Experienced Team: The company should have a seasoned team of experts who understand the nuances of various payer requirements and are well-versed in platforms like CAQH.
- Meeting Deadlines: The ability to meet deadlines and provide status reports is a non-negotiable quality. Your partner should be proactive in their communication and transparent about the process.
By entrusting your credentialing to an expert team, you free up your internal staff to focus on patient care and other revenue-generating activities, such as healthcare marketing and patient relations. It’s an investment that pays for itself many times over in saved time, prevented denials, and a steady revenue stream. For a comprehensive look at how a service can help, check out our guide on hiring an insurance credentialing service.
Frequently Asked Questions About Credentialing Costs
For more information, please visit our physician credentialing FAQ page.
The full credentialing process can take anywhere from 90 to 180 days, depending on the payer, state regulations, and the completeness of the provider's application. Delays can occur due to incomplete applications, slow payer responses, or missing documentation. An experienced service can significantly expedite this by ensuring all paperwork is accurate and by proactively following up.
Credentialing is the initial process of verifying a new provider's qualifications to enroll them with an insurance company. Re-credentialing is the process of re-verifying those same qualifications on an ongoing basis, typically every 3 to 5 years, to ensure the provider remains in good standing. Both are mandatory and require careful management to avoid billing interruptions.
If you choose the right partner, you shouldn't have to. A core function of a quality outsourced service is to manage and track document expirations for you, ensuring that everything from your medical license to your malpractice insurance is renewed on time. This proactive approach is a major benefit of outsourcing and saves you significant administrative time and risk.
Absolutely. Medicare enrollment, including applications like the CMS-855, can be particularly complex and time-consuming. Rxcredentialing has extensive experience with these applications. You can also review our ultimate guide on how to file your Medicare enrollment application for more information.
Final Words: Your Path to a Profitable Practice
The cost of medical credentialing is a significant factor in your practice's financial health, but it's a cost that can be controlled and optimized with the right strategy. While doing it yourself might seem appealing on the surface, the potential for costly mistakes and the immense time investment often make it the more expensive option in the long run. The true value lies not in saving a few dollars upfront but in the long-term efficiency and revenue security that a professional service provides.
Choosing the right physician credentialing service company to outsource is the best way to get the most out of your investment. It allows you to leverage expertise, scale your operations, and focus on what truly matters—your patients. We encourage you to explore our full suite of services, from medical licensing to A/R recovery, to build a practice that is both resilient and profitable.